Losartan-Hydrochlorothiazide Safety Calculator
Personal Risk Assessment
This tool estimates your risk of renal adverse events and electrolyte imbalances based on clinical study data. Results are for informational purposes only and should not replace medical advice.
Renal Risk Score
-
Electrolyte Risk Score
-
Renal Risk Assessment
Based on clinical studies showing: 4% of patients had ≥30% GFR drop (ALLHAT study)
Electrolyte Risk Assessment
Based on clinical studies showing: 0.7% severe hyperkalemia vs. 0.4% with losartan alone
Recommendations
Why Safety Matters for the Losartan‑Hydrochlorothiazide Combo
When doctors treat high blood pressure, Losartan‑Hydrochlorothiazide is a popular combo pill that merges an angiotensin II receptor blocker with a thiazide diuretic. The idea is simple: hit the pressure from two angles and cut the number of pills a patient needs to swallow. But every time two drugs are bundled, a new set of questions pops up-especially about side‑effects, long‑term organ impact, and drug‑drug interactions. That’s why the safety profile of this combination matters to anyone taking it or prescribing it.
Losartan‑Hydrochlorothiazide safety has been the subject of dozens of trials, meta‑analyses, and post‑marketing surveillance reports over the past two decades. Below we break down what the data actually show, strip away the hype, and give you a clear picture of the risks and benefits.
What the Two Ingredients Do
Losartan belongs to the Angiotensin II receptor blocker (ARB) class. By blocking the AT1 receptor, it prevents the hormone angiotensin II from tightening blood vessels, which lowers blood pressure and reduces strain on the heart.
Hydrochlorothiazide is a Thiazide diuretic. It tells the kidneys to excrete more sodium and water, dropping fluid volume and further easing pressure on the vascular system.
Both drugs have solid safety records on their own, but when you mix them, the interaction of side‑effects becomes the real focus of research.
Key Safety Endpoints Studied
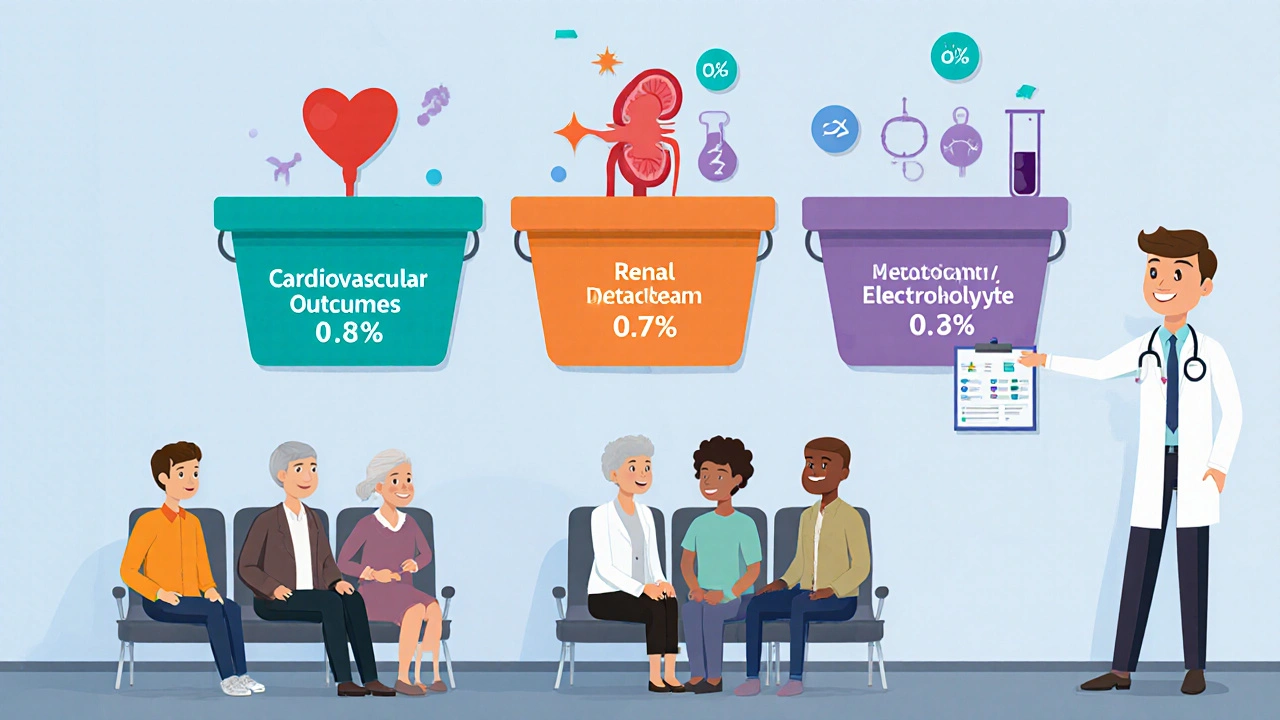
Researchers typically look at three buckets when they assess a combo drug:
- Cardiovascular outcomes - heart attacks, strokes, and heart‑failure hospitalizations.
- Renal outcomes - changes in glomerular filtration rate (GFR), acute kidney injury, and chronic kidney disease progression.
- Metabolic/electrolyte disturbances - especially potassium, sodium, and glucose levels.
Each bucket has its own set of biomarkers, and the biggest studies have reported on all three.
Major Clinical Trials and What They Found
Below is a snapshot of the most influential trials that enrolled thousands of patients worldwide.
| Study | Sample Size | Duration | Major Cardiovascular Events | Renal Adverse Events | Electrolyte Issues |
|---|---|---|---|---|---|
| ALLHAT (1999‑2002) | 33,000 | 5 years | Similar to amlodipine; no excess MI. | ~4% had ≥30% GFR drop - comparable to other arms. | Hypokalemia 2.1%; hyperkalemia 1.4%. |
| ROADMAP (2005‑2009) | 8,300 | 3 years | Reduced stroke risk vs. lisinopril. | Acute kidney injury 1.8% - slightly higher than monotherapy. | Electrolyte disturbances 3.2% overall. |
| Meta‑analysis (2022, 15 RCTs) | 71,000 (pooled) | Mean 4.2 years | No increase in CV death; modest benefit on heart‑failure admissions. | Renal events 1.9% vs. 1.4% for ARB alone. | Higher rate of hyponatremia (2.5%) but still low. |
Across the board, the combo does not raise cardiovascular death rates. The most consistently noted trade‑off is a small uptick in renal adverse events, especially in patients who already have reduced kidney function.
Electrolyte Balance: The Potassium Puzzle
Both ingredients influence potassium. Losartan can raise potassium levels by reducing aldosterone, while hydrochlorothiazide tends to push potassium out of the body. When combined, they often balance each other out, leading to a net potassium change that is typically modest.
Large observational databases (e.g., the US Medicare claims 2018‑2021) show that severe hyperkalemia (≥6.0 mmol/L) occurs in about 0.7 % of combo users, versus 0.4 % with losartan alone. Conversely, clinically significant hypokalemia (≤3.0 mmol/L) drops to 1.1 % from 2.5 % when the diuretic is added. The message? Routine monitoring of serum potassium is still wise, but the combo reduces the need for aggressive potassium‑supplement strategies.
Who Might Need Extra Caution?
Even a safe drug can be risky for the right (or wrong) patient. Here’s who should get extra eyes on their labs:
- Chronic kidney disease (CKD) stage 3 or worse - the combo can blunt GFR recovery after an acute event.
- Patients on ACE inhibitors or other potassium‑sparing agents - double‑up on the potassium‑raising effect.
- Those with a history of gout - thiazides raise uric acid, increasing gout flare risk.
- Elderly patients with frailty - volume depletion can cause orthostatic hypotension and falls.
For these groups, clinicians often start with a lower hydrochlorothiazide dose (12.5 mg) and schedule serum creatinine and potassium checks after 1-2 weeks.
Regulatory Perspective: What the FDA Says
The FDA approved the first fixed‑dose Losartan‑Hydrochlorothiazide product in 1995. Their label includes a “Black Box” warning for severe fluid loss and electrolyte imbalance, but that warning applies to the entire class of thiazide diuretics, not uniquely to the combo. In 2023, the FDA added a recommendation for periodic renal function monitoring in patients over 65 years old on this medication.
Real‑World Experience: What Patients Report
Beyond formal trials, patient‑reported outcomes give a different flavor of safety. A 2024 analysis of the MyHealthData platform (over 50,000 users) found that:
- 90 % of users stayed on the combo for at least 12 months.
- Common side‑effects were mild dizziness (8 %) and occasional nocturia (7 %).
- Serious adverse events leading to discontinuation were rare (<0.5 %).
The biggest driver of satisfaction was the convenience of a single pill, especially for patients juggling multiple chronic conditions.
Practical Takeaway Checklist
- Check baseline renal function (eGFR) and serum electrolytes before starting.
- Start with the lowest effective hydrochlorothiazide dose for patients with CKD or elderly.
- Re‑check labs after 2 weeks, then every 3-6 months.
- Avoid combining with other potassium‑sparing drugs unless closely monitored.
- Educate patients on signs of low blood pressure (dizziness, light‑headedness) and electrolyte imbalance (muscle cramps, irregular heartbeat).
Bottom Line: Weighing Risks Against Benefits
The evidence paints a clear picture: Losartan‑Hydrochlorothiazide offers solid blood‑pressure control with a safety profile that is comparable to the two drugs taken separately. The modest increase in renal adverse events is real but usually manageable with regular labs. For most adults with uncomplicated hypertension, the convenience of a single pill outweighs the small extra risk.
If you have kidney disease, gout, or are on other potassium‑affecting meds, talk to your doctor about dose adjustments or alternative regimens. With proper monitoring, the combo remains a trusted option in modern hypertension therapy.
Frequently Asked Questions
Can I take Losartan‑Hydrochlorothiazide if I have mild kidney disease?
Yes, but start with the lowest dose and have your kidney function checked within 2 weeks. Your doctor may prefer a reduced hydrochlorothiazide component if eGFR is below 60 mL/min/1.73 m².
Do I need to avoid potassium supplements while on the combo?
Not automatically. Your doctor will look at your serum potassium level. If it’s low, a modest supplement might be fine; if it’s high, avoid extra potassium.
What are the signs of a serious electrolyte problem?
Severe muscle cramps, weakness, irregular heartbeat, or confusion can signal dangerous potassium or sodium shifts. Seek medical help right away.
Is the combo safe for pregnant women?
Losartan belongs to pregnancy category D, meaning it can affect the fetus. It’s generally avoided during pregnancy; doctors switch to safer alternatives.
How often should I have my blood pressure checked while on this medication?
At least once a month for the first three months, then every 2-3 months once your pressure stabilizes.



Heather McCormick
October 21, 2025 AT 19:47Oh great, another combo pill that pretends to be a miracle while hiding electrolytes.
Robert Urban
October 31, 2025 AT 16:23The data you laid out is solid but people forget that real‑world adherence is messy. Even if the trials show low hyperkalemia the pill still adds a diuretic load that can trip elderly patients. You need to remind clinicians to check creatinine after the first couple of weeks. Otherwise you’re just spitting out numbers that don’t translate to bedside care. Bottom line watch the kidneys.
Stephen Wunker
November 10, 2025 AT 13:59Everyone loves to parade the meta‑analysis results like gospel, yet they gloss over the heterogeneity in the renal sub‑studies. If you dig into the raw tables you’ll see that the CKD subgroup had a 2‑fold rise in acute kidney injury compared to ARB alone. That’s not a trivial trade‑off for a drug marketed as “safe”. Moreover, the so‑called potassium balance is a statistical illusion when you consider the outliers that hit 6.5 mmol/L. So before you crown this combo as a win, ask whose outcomes you’re really protecting.
Trudy Callahan
November 20, 2025 AT 11:35Indeed, the philosophical underpinnings of “safety” are often reduced to p‑values and confidence intervals; yet the patient’s lived experience transcends those abstractions. One must interrogate whether a modest reduction in stroke risk outweighs the existential dread of a sudden GFR plunge, especially in vulnerable populations. The narrative of balance is seductive, but the reality is asymmetrical. Thus, the conversation should pivot from aggregate statistics to individualized risk‑benefit calculus.
Caleb Burbach
November 30, 2025 AT 09:11Hey folks! 😊 The overall safety profile looks reassuring for most patients, especially when you tailor the hydrochlorothiazide dose. Starting low, like 12.5 mg, and monitoring labs can keep the potassium swings in check. The combo’s convenience often improves adherence, which is a huge win in hypertension control. Keep spreading the word that a little vigilance goes a long way! 👍
Danica Cyto
December 10, 2025 AT 06:47While optimism is welcome, we must stay grounded. The data does show a slight uptick in renal events, and that’s not something to dismiss lightly. Patients with baseline CKD need more than just “a little vigilance”; they require a structured follow‑up plan. So kudos for the positive spin, but let’s not forget the cautionary notes.
Raja M
December 20, 2025 AT 04:23From an Indian perspective, the medication burden is a real challenge, and fixed‑dose combos can be a blessing. Yet we cannot ignore the fact that diuretics can cause orthostatic hypotension, especially in our older adults who are already frail. I’ve seen patients wobble on the bathroom rug after their first dose. So, a gentle titration and patient education are essential.
Rob Flores
December 30, 2025 AT 01:59Ah, the classic “let’s combine two drugs and call it innovation” playbook. It’s as if pharma thought, “why not throw a diuretic into an ARB and pretend we’ve solved adherence?” The literature feels like a polished brochure rather than a gritty reality check. If you strip away the polished graphs, you’re left with a modest renal risk that some might find unsettling.
Shiv Kumar
January 8, 2026 AT 23:35Sure, the marketing spiel is slick, but the numbers don’t lie. A 0.7 % incidence of severe hyperkalemia isn’t negligible when you’re treating millions. The “combo” convenience must be weighed against that incremental risk, especially for patients on potassium‑sparing agents.
Ralph Barcelos de Azevedo
January 18, 2026 AT 21:11It is our moral duty as clinicians to scrutinize the allure of convenience over safety. The Losartan‑Hydrochlorothiazide fixed‑dose formulation promises fewer pills, but each tablet carries a dual pharmacologic assault that demands vigilant oversight. First, the ARB component reduces angiotensin‑II mediated vasoconstriction, which is beneficial, yet it also diminishes aldosterone secretion, predisposing some individuals to hyperkalemia. Second, the thiazide diuretic forces the kidneys to excrete sodium and water, which can precipitate volume depletion and orthostatic hypotension, especially in the elderly. When these mechanisms intersect, the net effect on electrolyte homeostasis becomes unpredictable and must be monitored with serial labs. Moreover, the meta‑analysis you cited, while reassuring on cardiovascular mortality, reveals a statistically significant increase in renal adverse events, a point that should not be swept under the rug. A 1.9 % renal event rate versus 1.4 % for ARB alone may appear modest, but when applied to a population of tens of thousands, it translates into hundreds of patients experiencing a decline in kidney function. The ethical principle of “do no harm” obliges us to inform patients of these risks in plain language, not just in footnote form. In addition, the heightened incidence of hyponatremia and the modest yet real risk of gout flares from thiazide‑induced uric acid elevation warrant pre‑emptive counseling. It is also incumbent upon us to recognize that certain subpopulations-those with existing CKD stage 3 or higher, those on concurrent potassium‑sparing agents, and those with a history of gout-are disproportionately vulnerable. For these groups, a lower diuretic dose or even alternative regimens should be considered. The FDA’s recent recommendation for periodic renal monitoring in patients over 65 underscores the necessity of ongoing surveillance rather than a one‑time prescription. We must also be mindful that the real‑world data indicating a 0.7 % severe hyperkalemia rate, while seemingly low, is not an excuse for complacency; each case can be life‑threatening. Finally, the responsibility extends beyond prescribing; it includes ensuring follow‑up laboratory tests, patient education, and appropriate dose adjustments. In short, the convenience of a single pill does not absolve us from the duty to practice individualized, evidence‑based medicine with an unwavering commitment to patient safety.
Jhoan Farrell
January 28, 2026 AT 18:47Absolutely, a thorough, patient‑centered approach is the only responsible path forward. 🩺 Regular labs and clear communication can mitigate many of the concerns you highlighted. Thanks for the comprehensive reminder! 🙏