HIV Medication & Antibiotic Interaction Checker
Select your HIV medication and antibiotic to see interaction details.
When someone with HIV needs an antibiotic, it’s not as simple as picking up a prescription. The medicines that keep HIV under control can clash dangerously with common antibiotics - and these clashes aren’t always obvious. A 2023 study found that 41% of hospital admissions for HIV patients involved harmful drug interactions, and more than 2 out of 5 of those involved antibiotics mixed with antiretrovirals. This isn’t rare. Nearly 70% of people living with HIV take at least one antibiotic each year, often for pneumonia, urinary infections, or skin infections. If you’re on HIV meds and need an antibiotic, understanding these interactions isn’t optional - it’s lifesaving.
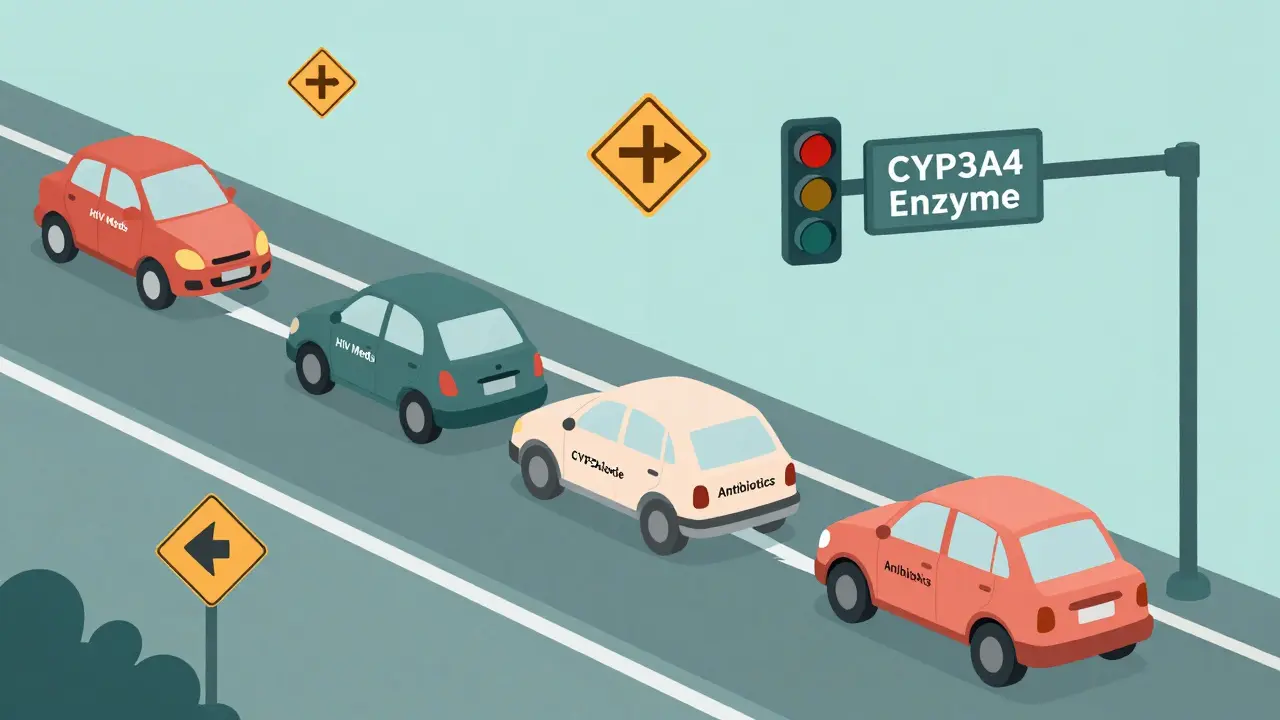
Why HIV Meds and Antibiotics Don’t Play Nice
The problem starts with how your body breaks down drugs. Most HIV medications and many antibiotics are processed by the same system: the cytochrome P450 enzyme system, especially the CYP3A4 enzyme. Think of it like a busy highway. If one drug slows down traffic (inhibits CYP3A4), other drugs pile up and flood your bloodstream. If another drug speeds things up (induces CYP3A4), the drugs get flushed out too fast and stop working.
Not all HIV drugs are the same. Some barely touch this system. Others? They’re heavy traffic controllers.
- NRTIs (like tenofovir and emtricitabine) and INSTIs (like dolutegravir and bictegravir) mostly avoid CYP3A4. They’re safer when paired with antibiotics.
- Boosted PIs (like darunavir/ritonavir or atazanavir/cobicistat) are strong CYP3A4 inhibitors. They slow down the breakdown of antibiotics, making them build up to toxic levels.
- NNRTIs (like efavirenz and rilpivirine) can both inhibit and induce CYP3A4 - unpredictable behavior that makes dosing tricky.
- Maraviroc (a CCR5 antagonist) also rides on CYP3A4 and can cause dangerous spikes in antibiotic levels.
Meanwhile, antibiotics like clarithromycin, azithromycin, rifampin, and fluoroquinolones each interact differently. Some are metabolized by CYP3A4. Others damage your kidneys alongside tenofovir. The combination isn’t random - it’s predictable, but only if you know the rules.
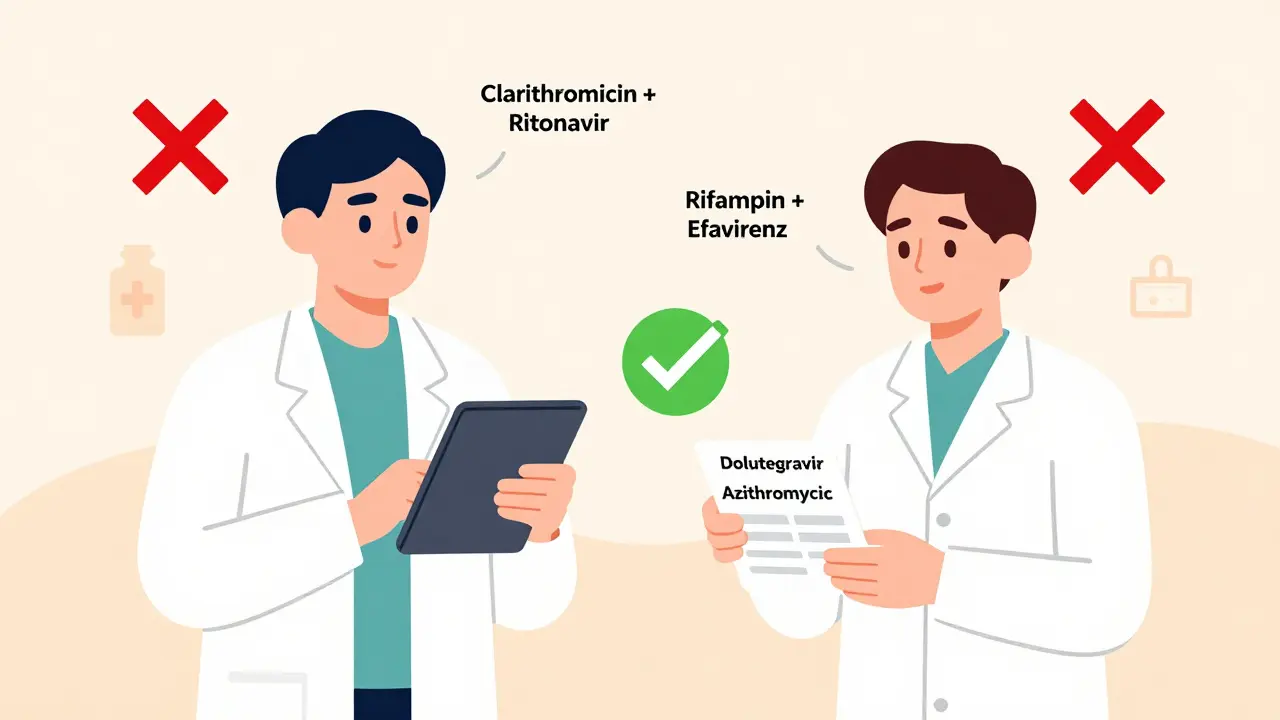
High-Risk Antibiotics and What to Do Instead
Not all antibiotics are equal when paired with HIV meds. Some are red flags. Others are safe bets. Here’s what the data says.
| Antibiotic | Problem with HIV Meds | Recommended Alternative | Why It’s Safer |
|---|---|---|---|
| Clarithromycin | Increases levels by 60-82% with boosted PIs | Azithromycin | Not metabolized by CYP3A4; no dose adjustment needed |
| Rifampin | Reduces PI and NNRTI levels by up to 80% | Rifabutin | Less potent inducer; can be dosed at 150mg every other day with boosted PIs |
| Tenofovir + Fluoroquinolones | 3.2x higher risk of kidney injury | Nitrofurantoin | No additive kidney toxicity; safe with dolutegravir or bictegravir |
| Voriconazole | Increases levels with cobicistat; risk of liver toxicity | Posaconazole | Minimal interaction; no dose adjustment needed |
| Trimethoprim-sulfamethoxazole | Can raise potassium levels with dolutegravir | Monitor electrolytes | Still usable with blood tests; avoid if already on potassium-sparing meds |
For example, if you’re on darunavir/ritonavir and get pneumonia, clarithromycin might be the go-to choice - but it’s dangerous. Azithromycin is just as effective for pneumonia and doesn’t interfere. The same goes for tuberculosis: rifampin is a standard treatment, but it wipes out HIV meds. Rifabutin is the workaround - but even then, doses must be cut in half and monitored.
What About Newer HIV Drugs?
Not all HIV medications are created equal. The newer ones were designed with fewer interactions in mind.
Dolutegravir and bictegravir - the backbone of many modern regimens - have minimal CYP450 activity. They’re the safest anchors when antibiotics are needed. A 2023 review showed that patients on dolutegravir-based therapy had 70% fewer significant drug interactions compared to those on boosted PIs.
Even newer are the long-acting injectables: cabotegravir and rilpivirine. They’re given every month or two. But here’s the catch: because they stick around for weeks, any interaction doesn’t just last days - it lasts months. If you stop an antibiotic that was interacting with cabotegravir, the effects can linger for over 50 days. That means even after the antibiotic is gone, your body is still at risk.
Then there’s lenacapavir, a capsid inhibitor approved in 2022. It doesn’t touch CYP3A4 at all. It’s a game-changer for people who need multiple antibiotics over time. And the next wave? Islatravir, still in trials, shows only a 7% change in levels when mixed with clarithromycin - a tiny blip compared to the 80% spikes seen with older drugs.
The Real Danger: Hidden Risks and Silent Failures
Some interactions don’t cause immediate symptoms. They quietly break down your treatment.
If an antibiotic reduces your HIV drug levels too much, the virus can start replicating again. You might not feel sick. Your viral load test might not spike right away. But resistance builds. And once you develop resistance to one drug, it can wipe out entire classes. That means fewer options next time.
On the flip side, if an antibiotic builds up too high - like clarithromycin with a boosted PI - you risk serious side effects: heart rhythm problems, liver damage, or even sudden death. The FDA has issued warnings for this exact scenario.
And it’s not just about prescriptions. Over-the-counter herbs like St. John’s Wort? It’s a CYP3A4 inducer. It can slash your HIV drug levels by 50%. Even common painkillers like ibuprofen can interfere with tenofovir in high doses. Your pharmacist needs to know everything you’re taking - not just the pills, but the supplements, the teas, the recreational drugs.
What You Should Do Right Now
Here’s what works in real life - not theory.
- Always check before starting any new drug. Use the University of Liverpool HIV Drug Interactions Checker. It’s free, updated weekly, and used by clinics worldwide. It flagged over 400 interactions as of January 2024.
- Ask your doctor to use INSTI-based regimens (dolutegravir or bictegravir) if you’re on multiple antibiotics. They’re the safest.
- Never switch antibiotics without review. If your primary care provider prescribes clarithromycin, ask: "Is this safe with my HIV meds?" If they don’t know, push for a pharmacist consult.
- Track your viral load. If you start a new antibiotic, get your viral load tested 4-6 weeks later. A sudden rise means an interaction is happening.
- Keep a full list of everything you take. Include vitamins, supplements, and herbal products. Show it to every provider - even the dentist.
For example, if you’re on dolutegravir and get a UTI, nitrofurantoin is fine. But if you’re on a boosted PI and need the same drug, you might need to switch to cephalexin. It’s not about which drug is "stronger." It’s about which combo won’t break your treatment.
What’s Changing in 2025 and Beyond
Big changes are coming. The NIH just launched a $15.7 million project to build personalized dosing algorithms using your genes and current meds. Imagine a tool that says: "Based on your HIV regimen and kidney function, here’s the exact antibiotic dose you need." That’s the future.
The Liverpool database, now using machine learning, predicts new interactions before they’re even published. And by late 2025, major drug databases (Micromedex, Drugs.com, Lexicomp) plan to finally align their interaction ratings - so a "contraindicated" flag means the same thing everywhere.
For now, though, you can’t wait. The tools exist. The data is clear. And the risks are real.
Can I take antibiotics while on HIV meds?
Yes, but not all antibiotics are safe. Many can dangerously raise or lower your HIV medication levels. Always check for interactions before starting any antibiotic. INSTI-based regimens like dolutegravir or bictegravir are the safest options when antibiotics are needed.
Is azithromycin safe with HIV meds?
Azithromycin is one of the safest antibiotics for people on HIV meds. It doesn’t rely on the CYP3A4 enzyme, so it doesn’t interfere with boosted PIs, NNRTIs, or INSTIs. It’s often the first choice for pneumonia or sinus infections in HIV patients.
Why is rifampin dangerous with HIV drugs?
Rifampin is a powerful inducer of CYP3A4 - it speeds up the breakdown of most HIV medications. This can drop drug levels by up to 80%, leading to treatment failure and drug resistance. It’s contraindicated with all boosted PIs and most NNRTIs. Rifabutin is the safer alternative, but even then, doses must be adjusted.
Can I use St. John’s Wort with my HIV meds?
No. St. John’s Wort is a strong CYP3A4 inducer and can cut HIV drug levels in half. Even one dose can trigger viral rebound. Avoid it completely if you’re on any antiretroviral therapy.
What should I do if I’m on tenofovir and need an antibiotic?
Avoid fluoroquinolones (like ciprofloxacin or levofloxacin) - they raise the risk of kidney injury by over 3 times. Use nitrofurantoin for UTIs, or amoxicillin/clavulanate for respiratory infections. Always check kidney function before and after starting the antibiotic.




John Watts
February 9, 2026 AT 23:30Man, this post is a game-changer. I’ve been on dolutegravir for years and just last month my doc prescribed azithromycin for a sinus infection. No one even mentioned checking interactions - I thought all antibiotics were "safe" if you’re stable. Turns out I was lucky. Now I keep the Liverpool checker bookmarked and show it to every new provider. Seriously, if you’re on HIV meds, treat drug interactions like a bomb squad - assume everything’s dangerous until proven otherwise.
Camille Hall
February 9, 2026 AT 23:32This is so important. I work in a clinic and see patients get antibiotics all the time without any thought to their ART. One woman on atazanavir/cobicistat was given clarithromycin for bronchitis - her liver enzymes went through the roof. We had to admit her. We need mandatory pharmacist reviews for every HIV patient getting a new med. It’s not optional. It’s basic safety.
Ritteka Goyal
February 10, 2026 AT 06:18OMG this is so true in India too!! I have a cousin on ART and he took ciprofloxacin for UTI and got super dizzy and vomited for 3 days!! Doctors here dont even know about this!! We need more awareness!! I read this article and shared with 5 friends already!! Also, why dont we have a simple app that scans your pills and tells you if they clash?? Like a barcode scanner for HIV meds and antibiotics?? India needs this!! Please someone build it!!
Monica Warnick
February 11, 2026 AT 21:40Okay but let’s be real - most people on HIV meds are just too scared to ask questions. I’ve seen it. You go to your doctor, they say "take this antibiotic," and you nod because you’re terrified they’ll think you’re difficult. And then you Google it later and panic because you’ve been taking rifampin for TB for 6 months with your PI and now your viral load is creeping up. This post should be mandatory reading for every HIV patient. And every GP. And every ER nurse. And your aunt who gives you herbal tea. Everyone.
Chelsea Deflyss
February 12, 2026 AT 17:52St. John’s Wort? Really? Like, who even uses that anymore? And why are people still taking it with HIV meds? It’s not 2005. If you’re taking supplements without checking interactions, you’re just playing Russian roulette with your life. And don’t even get me started on people who think "natural" means "safe."
Tricia O'Sullivan
February 13, 2026 AT 09:52Thank you for this comprehensive and clinically grounded overview. I am a pharmacist in Dublin and encounter these interactions weekly. The Liverpool database is indeed indispensable. I would only add that for long-acting injectables, the window of interaction risk extends far beyond the cessation of the co-administered agent. A patient on cabotegravir/rilpivirine who received a single dose of rifampin remains at risk for viral rebound for over 60 days. This requires proactive monitoring, not reactive.
Brandon Osborne
February 13, 2026 AT 16:12YOU THINK THIS IS BAD? I’M ON DORAVIRINE AND MY DOCTOR GAVE ME FLUOXETINE FOR DEPRESSION. 3 WEEKS LATER I WAS IN THE ER WITH A 104 FEVER AND MY KIDNEYS WERE SHUTTING DOWN. THEY SAID IT WAS "COINCIDENCE." COINCIDENCE?? I WAS ON 3 DRUGS THAT ALL TALK TO CYP3A4. I’M STILL SCARED TO TAKE ANYTHING NOW. MY DOCTOR NEVER ASKED ME WHAT I WAS ON. NEVER. I HAD TO GOOGLE IT MYSELF. THIS IS A SCANDAL. PEOPLE ARE DYING BECAUSE DOCTORS DON’T CARE.
Lyle Whyatt
February 15, 2026 AT 14:19As someone who’s been on ART for 15 years and has had pneumonia twice, I can tell you - azithromycin is the MVP. I used to get clarithromycin because it was "stronger." Turned out it was just more dangerous. Now I ask for azithro by name. My pharmacist even has a sticky note on my file: "Ask for azithromycin." I’ve also switched to bictegravir because my old regimen with boosted PI was a minefield. If you’re on a PI, ask if you can switch. It’s not a betrayal of your old treatment - it’s upgrading your safety protocol.
Ken Cooper
February 16, 2026 AT 19:47Wait wait wait - so if I’m on dolutegravir and I get a UTI, nitrofurantoin is fine? But if I’m on a boosted PI, I need cephalexin? And what about amoxicillin? Is that safe? I’m confused. Also, does this apply to over-the-counter stuff like cranberry pills? And what about probiotics? Do they interfere? I need a flowchart. A real one. With arrows. And emojis. I’m not a doctor, but I’ve been reading this stuff for 10 years. I just want to not die.
Jacob den Hollander
February 18, 2026 AT 13:53Thank you for this. I’m a nurse who works with HIV patients, and I’ve seen too many cases where antibiotics were prescribed without checking interactions. One patient on darunavir/ritonavir got clarithromycin for a sinus infection - ended up in the ICU with QT prolongation. We almost lost him. Since then, I’ve started a checklist: 1) What ART? 2) What antibiotic? 3) Check Liverpool. 4) Consult pharmacy. 5) Educate patient. It’s not extra work - it’s basic care. I wish every provider had to do this before prescribing. And yes, I’ve started handing out laminated cards with the top 5 dangerous combos and their alternatives. It’s small, but it saves lives.