
Ever bought an OTC painkiller for a headache, only to find it didn’t help? Or taken a prescription pill your doctor gave you last year for heartburn, only to realize it’s now sitting on the shelf because you can buy the same thing at the grocery store? You’re not alone. The line between what you can grab off the shelf and what needs a doctor’s signature is blurrier than ever - and getting it wrong can cost you time, money, or worse.
What’s the Real Difference Between OTC and Prescription Medications?
It’s not just about who writes the script. OTC medications are designed for self-treatment of minor, clearly identifiable issues. Prescription drugs are for conditions that need professional diagnosis, ongoing monitoring, or stronger doses. The FDA regulates both, but in totally different ways. OTC drugs follow a set of approved formulas called monographs - think of them as recipes that have been tested and approved for safety. Prescription drugs go through a much longer, more expensive approval process called the New Drug Application (NDA). That’s why you’ll see the same active ingredient in both forms, but with different strengths, timing, or delivery methods.
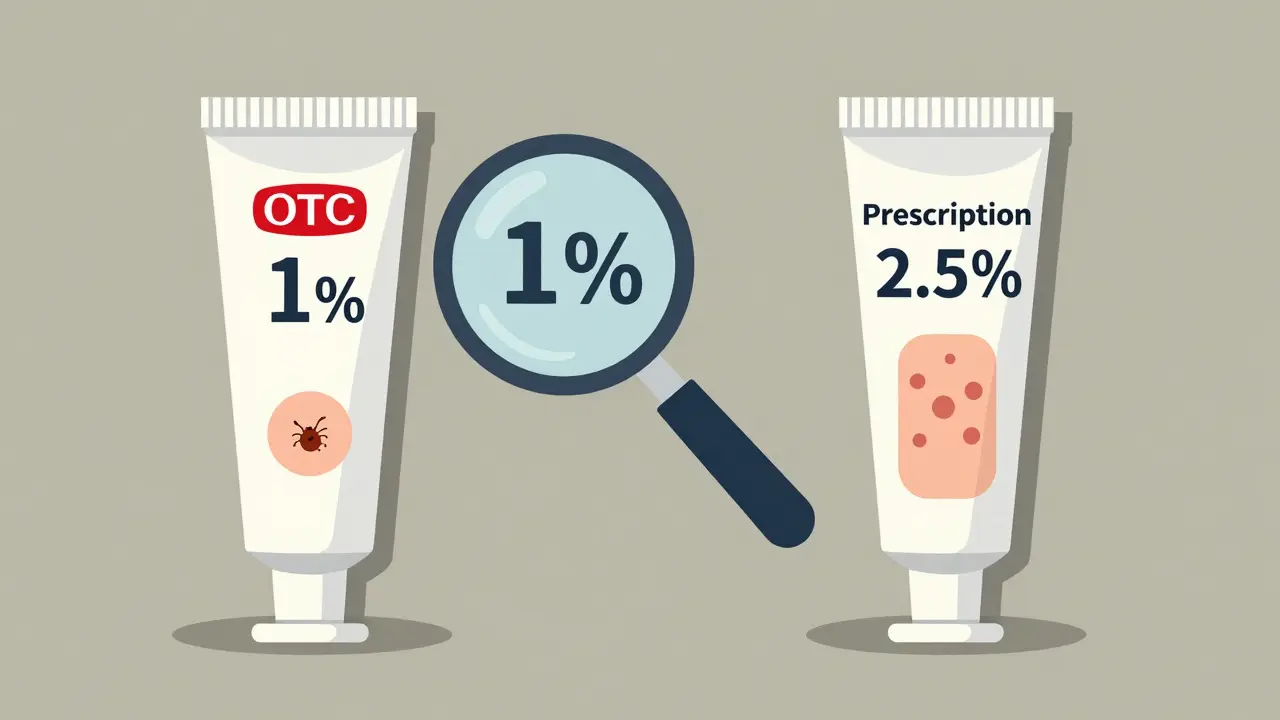
Take hydrocortisone cream. The OTC version is 1% - fine for a small rash or bug bite. But if you’ve got a stubborn eczema flare-up, your doctor might prescribe the 2.5% version. Same ingredient. Different power. Same with ibuprofen: OTC is 200 mg per tablet. Prescription strength? Up to 800 mg. You can’t just take four OTC pills to match it - that’s how stomach bleeds happen.
When OTC Is the Smart Choice
OTC meds shine when your symptoms are mild, short-term, and familiar. If you’ve had a headache like this before, and it’s not getting worse, an OTC pain reliever is perfectly reasonable. Same for a runny nose from a cold, mild heartburn after spicy food, or seasonal allergies that come every spring.
Here’s what works well with OTC options:
- Headaches: Acetaminophen (Tylenol), ibuprofen (Advil), or naproxen (Aleve). Combination products like Excedrin (which includes caffeine) can help with migraines if they’re mild and under 10 days a month.
- Allergies: Cetirizine (Zyrtec), loratadine (Claritin), or fexofenadine (Allegra). These start working in about an hour and don’t make you drowsy like older antihistamines.
- Heartburn: OTC esomeprazole (Nexium 24HR) or omeprazole (Prilosec OTC). These are proton pump inhibitors - they don’t give instant relief like Tums, but they reduce acid production over a few days.
- Minor aches and pains: Topical creams with menthol or capsaicin for sore muscles. OTC hydrocortisone for itchy skin.
One big myth? That OTC means cheap. Not always. A 100-tablet bottle of store-brand ibuprofen 200 mg costs around $4. Brand-name Advil? Around $15. But if you have Medicare Part D or private insurance, your prescription version of the same drug might be $5 with a copay. Always check.
When You Need a Prescription
OTC meds aren’t magic. If your symptoms don’t improve in 7-10 days, get worse, or start interfering with sleep, work, or daily life - it’s time to see a provider. Prescription medications fill gaps OTC drugs can’t reach.
Here’s when you shouldn’t try to self-treat:
- Chronic or severe migraines: OTC painkillers might dull the edge, but if you’re having more than 10 headache days a month, or your attacks come with nausea, light sensitivity, or last over 24 hours, you need something stronger. Triptans like sumatriptan (Imitrex) or rizatriptan (Maxalt) work fast and target the root cause. OTC versions simply don’t have the punch.
- High blood pressure or diabetes: These aren’t conditions you diagnose yourself. You need regular monitoring, lab tests, and adjustments based on your body’s response. No OTC pill fixes this.
- Depression, anxiety, or insomnia: While melatonin or valerian root are OTC, they’re not replacements for antidepressants or sleep meds prescribed after a clinical evaluation.
- Chronic pain: If you’re taking ibuprofen daily for back or joint pain, you’re risking kidney damage or ulcers. A doctor can assess whether you need physical therapy, stronger anti-inflammatories, or even imaging to find the root cause.
And here’s something many don’t realize: some OTC meds are just weaker versions of prescription drugs. Take adapalene gel for acne. It was once prescription-only. Now you can buy it OTC as Differin. But the prescription version might be combined with antibiotics or retinoids for stubborn cases. Same ingredient. Different strategy.
The Rx-to-OTC Switch: Why It’s Happening
Over the last 15 years, more prescription drugs have made the leap to OTC. Fexofenadine (Allegra), esomeprazole (Nexium), and now even epinephrine auto-injectors (EpiPen) are available without a prescription. Why? Because safety data showed they’re low-risk when used correctly, and people want faster access.
The FDA’s OTC Monograph Reform under the CARES Act of 2020 made this process faster and more flexible. The goal? Empower people to manage common conditions without a doctor’s visit - as long as they know how to use the product safely.
But here’s the catch: just because it’s OTC doesn’t mean it’s harmless. People often think, “It’s on the shelf, so it’s safe.” Not true. Taking too much acetaminophen can cause liver failure. Mixing NSAIDs with blood thinners can cause bleeding. Using OTC nasal sprays for more than three days can rebound congestion. Read the label. Know the limits.
What Pharmacists Know That You Don’t
Most people walk into a pharmacy and grab what they think they need. But pharmacists are trained to spot red flags. Eighty-nine percent of community pharmacists say they regularly counsel patients on whether an OTC option is appropriate - or if they need to see a doctor.
Here’s what they look for:
- Are you taking multiple OTC meds that interact? (Like ibuprofen + aspirin + cold syrup - all with NSAIDs)
- Are you using an OTC version of a drug you used to get by prescription, but at the wrong dose?
- Are you ignoring symptoms that should’ve been checked weeks ago?
Don’t be shy. Ask the pharmacist: “Is this safe for me to take with my other meds?” or “Should I be seeing a doctor instead?” They’re there to help - not to upsell.

What’s Coming Next
The OTC landscape is changing fast. By 2030, experts predict 20-25 more prescription drugs will become available over the counter. The next big targets? Birth control pills, asthma inhalers, and even some antidepressants.
Why? Because access matters. But so does safety. New labeling rules that took effect in January 2024 require clearer dosage instructions, interaction warnings, and side effect info on all OTC packaging. That’s a good thing. It means you’ll have fewer surprises.
And here’s a trend you’ll see more of: dual-formulation options. For example, migraine meds might come in both OTC (slow-release, for mild cases) and prescription (fast-acting, for severe attacks). The same drug. Two different tools for two different needs.
Final Rule of Thumb
Ask yourself these three questions before reaching for an OTC bottle:
- Is this a new symptom? If you’ve never felt this way before - especially if it’s sudden or severe - don’t guess. See a doctor.
- Is this getting worse or lasting longer than a week? OTC meds are for short-term relief. Not long-term fixes.
- Am I taking this because it’s cheaper or because it’s right for me? Sometimes, the prescription version is actually cheaper with insurance. Sometimes, the OTC version won’t touch your problem.
Medications aren’t snacks. They’re tools. And like any tool, using the wrong one - or using it the wrong way - can do more harm than good. Know your limits. Know your body. And when in doubt? Talk to a professional. It’s not weakness. It’s wisdom.
Can I just take more OTC pills if the first one doesn’t work?
No. Taking more than the recommended dose of OTC painkillers like acetaminophen or ibuprofen won’t make them work faster - it just increases your risk of liver damage, stomach bleeding, or kidney problems. If one dose doesn’t help, wait the full recommended time before taking another. If symptoms persist, see a doctor. More isn’t better.
Why does my OTC heartburn medicine take days to work?
OTC proton pump inhibitors like esomeprazole (Nexium 24HR) or omeprazole (Prilosec) reduce stomach acid production over time. They don’t neutralize acid like antacids (Tums, Rolaids) - they shut it down at the source. That’s why you might still feel discomfort the first day. Full effect usually takes 2-4 days. If you’re expecting instant relief, you’re using the wrong tool. For quick relief, use an antacid. For long-term control, stick with the PPI.
Is it safe to use OTC allergy meds every day?
Yes, for most people. Second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) are designed for daily use and don’t cause drowsiness. But if you’re taking them year-round and still have symptoms, you may have an underlying condition like nasal polyps or chronic sinusitis that needs medical attention. OTC meds treat symptoms - not causes.
Can I switch from a prescription drug to the OTC version?
Sometimes - but not always. For example, switching from prescription esomeprazole to OTC Nexium 24HR is fine if your condition is stable. But if you were on a higher dose or a combination drug (like esomeprazole with an antibiotic), the OTC version won’t be enough. Always check with your doctor or pharmacist before switching. Same active ingredient doesn’t mean same effect.
Why did the FDA approve OTC epinephrine?
Because anaphylaxis - a life-threatening allergic reaction - can happen anywhere, anytime. Previously, people had to carry a prescription EpiPen, which meant they needed a doctor’s visit every year to renew it. With OTC epinephrine, anyone can buy it without a script. It’s a public health win - especially for kids, travelers, or people without regular access to a doctor. But it’s not a replacement for emergency care. You still need to call 911 after using it.
For most common issues, OTC medications are safe, effective, and convenient. But they’re not a substitute for medical care when things get serious. Knowing when to use each - and when to ask for help - is the real skill.



Georgia Brach
December 24, 2025 AT 16:06The entire premise of this article assumes people are rational actors with access to healthcare. In reality, millions of Americans can't afford a doctor's visit but can afford a $4 bottle of ibuprofen. Calling OTC meds 'not a substitute for medical care' is a luxury argument from someone who's never had to choose between rent and a prescription.
Also, the FDA's OTC monograph reform? More like corporate lobbying disguised as public health policy. Big Pharma doesn't want you self-treating - they want you dependent on their overpriced branded versions, even if the active ingredient is identical.
And let's not pretend pharmacists are neutral advisors. They get commissions on certain OTC lines. Ask them why they push the $15 brand-name version over the $4 generic - they'll avoid the question.
siddharth tiwari
December 24, 2025 AT 16:33u think otc is safe? lol. i saw a guy in mumbai take 12 ibuprofen cause he thought 'more = better'. he died. now his kid is in orphanage. big pharma dont care. they sell pills. not care. government too. they just want you to buy more. even if u die. its all about money. no one care bout truth.
also why epinephrine otc? who gonna use it? rich people? no. poor people dont even have money for bus ticket to hospital. this is just trick. to make u feel safe. but u r not safe. ever think bout that?
Diana Alime
December 25, 2025 AT 02:00Okay but why is it that every time I try to use OTC heartburn meds, I end up feeling like I swallowed a live cactus for three days? And then I go to the doctor and they give me the exact same pill but it’s ‘prescription’ and suddenly it works? I’m not dumb. I know it’s the same chemical. Why do they make us pay more for the same thing just because it has a fancy label?
Also, I bought the OTC version of that acne gel and it did NOTHING. Then my dermatologist gave me the ‘prescription’ one and it burned my face off in two days. So… which one is the real one? I’m confused. And also mad. And also crying. Why is medicine so weird??
Also, I think my pharmacist hates me. She always sighs when I ask if the generic is the same. I’m not asking for a Nobel Prize. I just want to not get scammed.
Adarsh Dubey
December 26, 2025 AT 17:35This is a well-researched and balanced piece. The distinction between symptom management and disease treatment is critical, and too many people conflate the two. The rise of OTC access is a net positive, provided it’s paired with education.
I’ve seen patients in rural India self-medicate with antibiotics for viral infections - that’s the real danger. OTC doesn’t mean risk-free. It means responsibility. The key is not banning access, but improving literacy around usage.
Also, the point about pharmacists being underutilized is spot-on. They’re the most accessible healthcare professionals, yet most people treat them like cashiers. A simple question like ‘Is this right for me?’ could prevent serious harm.
Chris Buchanan
December 27, 2025 AT 17:53Ohhhhh so THAT’S why my ‘OTC migraine pill’ didn’t work? I thought I was just a failure at life. Turns out I just needed to pay $150 for a prescription that does the same thing but with a better label? Genius. Absolute genius.
And let’s talk about the ‘pharmacist advice’ - I asked mine if I could take my OTC painkiller with my blood pressure med. She said ‘probably fine’ and handed me a free sample of a $70 nasal spray. Thanks, Karen.
Look - I get it. OTC is great for when you’re not dying. But when you’re in pain and broke, the system is designed to make you feel guilty for trying to survive. So yeah - I’ll keep taking my $4 ibuprofen and ignoring the 12-page warning label. I’ve got bills to pay, not a medical degree.
Wilton Holliday
December 28, 2025 AT 07:27Love this breakdown. Seriously. So many people don’t realize that OTC doesn’t mean ‘safe for everyone’ - it means ‘safe for most people, if used correctly.’
And I’m so glad you mentioned the pharmacist. I used to be terrified to ask questions at the counter. Then one day I just said, ‘Hey, I’ve been taking this for three weeks. Is this still okay?’ They paused, looked at my med list, and said, ‘You’re mixing three NSAIDs. Stop. Now.’ Saved me from a GI bleed.
Don’t be shy. Pharmacists aren’t salespeople - they’re your secret healthcare weapon. And yes, the generic is almost always the same. Just check the active ingredient. Same molecule. Different price tag. 😊
Bret Freeman
December 29, 2025 AT 23:48Let me guess - you’re one of those people who thinks the FDA is some kind of benevolent guardian of truth. Newsflash: they’re a bureaucratic nightmare run by former pharmaceutical lobbyists. The ‘OTC switch’ isn’t about access - it’s about profit. Companies don’t want to pay for prescription patents anymore. So they slap a ‘new formula’ label on the same drug and charge you $20 more.
And don’t get me started on the ‘dual-formulation’ nonsense. It’s a scam. One pill for mild cases, another for severe? That’s not innovation - that’s price discrimination. You’re not getting two tools. You’re getting one tool and a middleman who wants your money.
Also, ‘read the label’? Sure. Except the label is written in 8-point font with 17 disclaimers and zero actual guidance on what ‘prolonged use’ means. Is that 7 days? 14? 30? No one knows. That’s not transparency. That’s legal cover.
And why is it that every time someone says ‘see a doctor,’ they’re really saying ‘pay me $300 for a 10-minute visit where you’ll get the same pill you could’ve bought for $4’? I’m tired of being gaslit by the healthcare industry.
Gray Dedoiko
December 30, 2025 AT 00:20I’ve been taking OTC ibuprofen for years for back pain. Didn’t think much of it until I started getting stomach cramps. My doctor said I was lucky I didn’t bleed out. Now I use a topical cream instead. It’s slower, but safer.
Point is - we all think we know what’s ‘minor.’ But your body doesn’t care if you think it’s ‘just a headache.’ It just reacts. I wish I’d listened earlier.
Also, the pharmacist who asked me if I was on any other meds? That was the first time anyone ever asked me that. I cried in the parking lot. Not because I was sick. Because I felt seen.
Don’t be afraid to ask. Even if it’s dumb. Even if you feel silly. Someone’s got your back if you just speak up.
Aurora Daisy
December 31, 2025 AT 01:11Oh, so now we’re trusting Americans to self-diagnose with OTC meds? Brilliant. Because clearly, the average American can’t tell the difference between a headache and a stroke. Next you’ll be selling insulin at Walmart and calling it ‘health empowerment.’
And let’s not forget the real issue - the U.S. healthcare system is so broken that people have to rely on OTC drugs because they can’t access care. This isn’t progress. It’s surrender.
Meanwhile, in the UK, we have the NHS. If you have heartburn, you go to your GP. If you need painkillers, you get them for free. No guessing. No risk. No corporate profit motive.
So yes - OTC is convenient. But it’s also a symptom of a system that failed its people. And you’re celebrating that? Disgraceful.
Paula Villete
January 1, 2026 AT 01:07There’s something deeply poetic about how we treat medicine like a grocery list. ‘I’ll take two of these, one of those, and maybe a little extra because why not?’
But here’s the truth - we’re not just buying pills. We’re buying peace of mind. And when the peace of mind doesn’t come, we feel stupid. Like we failed at being healthy.
What if the real problem isn’t the OTC vs. prescription divide? What if it’s that we’ve been taught to fix ourselves, not to ask for help?
I used to think seeing a doctor meant weakness. Now I know it’s the bravest thing you can do - admitting you don’t have all the answers. And that’s okay.
Also, typo: ‘proton pump inhibitors’ is hard to spell. I got it wrong twice. But I still took the pill. And I’m still here. So maybe that’s the point - we’re all just trying to survive, one typo at a time.
Katie Taylor
January 2, 2026 AT 19:09STOP IT. STOP JUSTIFYING OTC AS IF IT’S A RIGHT. People are dying because they think ‘it’s just a pill.’ I had a friend take 10 Advil for a headache. She went to the ER. Liver failure. Now she’s on a transplant list. All because someone told her it was ‘safe.’
And don’t give me that ‘pharmacist advice’ crap. My cousin went to CVS and asked if OTC melatonin was okay with her antidepressant. The pharmacist said ‘probably fine’ - then sold her a $20 vitamin bundle.
Stop romanticizing self-medication. It’s not empowerment. It’s a death sentence waiting to happen. And you’re all acting like it’s a lifestyle choice. It’s not. It’s negligence dressed up as convenience.
Isaac Bonillo Alcaina
January 3, 2026 AT 22:03Anyone who trusts OTC meds without a prescription is either naive or dangerously ignorant. You think the FDA is protecting you? They’re protecting Big Pharma’s bottom line. The same active ingredient? Same company. Same factory. Different bottle. Different price. Same risk.
And the ‘dual-formulation’ nonsense? That’s not innovation - that’s exploitation. You think you’re getting a choice? You’re getting a price tier. The rich get the fast-acting version. The poor get the slow-acting placebo with a warning label no one reads.
And don’t even get me started on the ‘pharmacist’ myth. They’re paid to upsell. They don’t care if you live or die. They care if you buy the $12 bottle instead of the $4.
You’re not empowered. You’re being milked. Wake up.
Bhargav Patel
January 5, 2026 AT 13:44Medication is not a consumer good. It is a biological intervention, and its use requires contextual understanding - not merely label reading. The OTC transition reflects a broader societal shift toward individual responsibility in health, yet without commensurate investment in public health literacy.
It is not sufficient to say, ‘read the label.’ One must understand pharmacokinetics, drug interactions, contraindications, and the physiological basis of one’s symptoms - knowledge not universally accessible.
The true challenge lies not in the availability of drugs, but in the absence of education. Without this, OTC access becomes a false promise - offering autonomy while obscuring risk.
Perhaps the next step should not be more OTC switches, but mandatory, standardized health literacy modules in secondary education. Not as a cure, but as a foundation.
Joe Jeter
January 6, 2026 AT 16:20Oh, so now the solution to healthcare inequality is to let people kill themselves with OTC drugs? Brilliant. Because clearly, the answer to ‘I can’t afford a doctor’ is ‘take more pills.’
And the ‘OTC epinephrine’ thing? You think a panic-stricken parent in a Walmart parking lot is going to use it correctly? Or are they just going to shake it like a soda can and then cry while their kid turns blue?
And why is it that every time someone says ‘ask your pharmacist,’ they mean ‘pay $15 for a 30-second conversation that ends with a coupon for a $70 nasal spray’?
This isn’t empowerment. It’s a trap. And you’re all too busy patting yourselves on the back to notice.
Paula Villete
January 8, 2026 AT 14:57Actually… I think the real issue isn’t OTC vs. prescription.
It’s that we’ve turned medicine into a transaction, not a conversation.
People don’t need more pills.
They need someone to listen.
That’s why I keep taking my $4 ibuprofen - because I don’t have time to sit in a waiting room for 3 hours just to be told ‘take two and call me in the morning.’
But I’d pay $100 for a 10-minute chat with someone who actually cares.
Not a pharmacist with a sales quota.
Not a doctor who’s running 20 minutes behind.
Just someone who says, ‘I see you. Let’s figure this out together.’
That’s the medicine I’m still waiting for.