
Why documenting generic substitutions isn’t optional - it’s essential
Every time a pharmacist swaps a brand-name drug for a generic version, they’re making a clinical decision. Not just a cost-saving one. And if that decision isn’t properly recorded, it can lead to serious consequences: wrong dosages, dangerous interactions, or even hospitalizations. In the U.S., nearly 90% of prescriptions are filled with generics when available. That’s a huge number. But behind every one of those substitutions is a paper trail - or, more often now, an electronic one - that must be complete, accurate, and timely.
What exactly counts as a generic substitution?
Generic substitution means dispensing a different brand or unbranded version of the drug that was originally prescribed. It’s not just swapping one pill for another that looks similar. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They also must prove bioequivalence - meaning the body absorbs the drug at the same rate and extent, within an 80-125% confidence range. This isn’t guesswork. It’s science. And the Orange Book, published by the FDA, is the official list that tells pharmacists which generics are approved as therapeutically equivalent.
State laws vary - and they matter more than you think
There’s no single federal rule forcing pharmacists to document every substitution. Instead, 50 different state laws do. Forty-three states require pharmacists to record the substitution on the prescription record. But what gets recorded? And when? That’s where it gets messy.
In 27 states, pharmacists can swap generics without asking the patient. In 14 states, they must get explicit consent. Nine states mix both rules. Oklahoma is one of the strictest - pharmacists can’t substitute unless the prescriber or patient gives direct permission, and that permission must be documented. California’s new law, SB 564, which took effect January 1, 2024, goes even further: substitutions must now be recorded in real time and made visible to the prescribing doctor through the electronic health record.
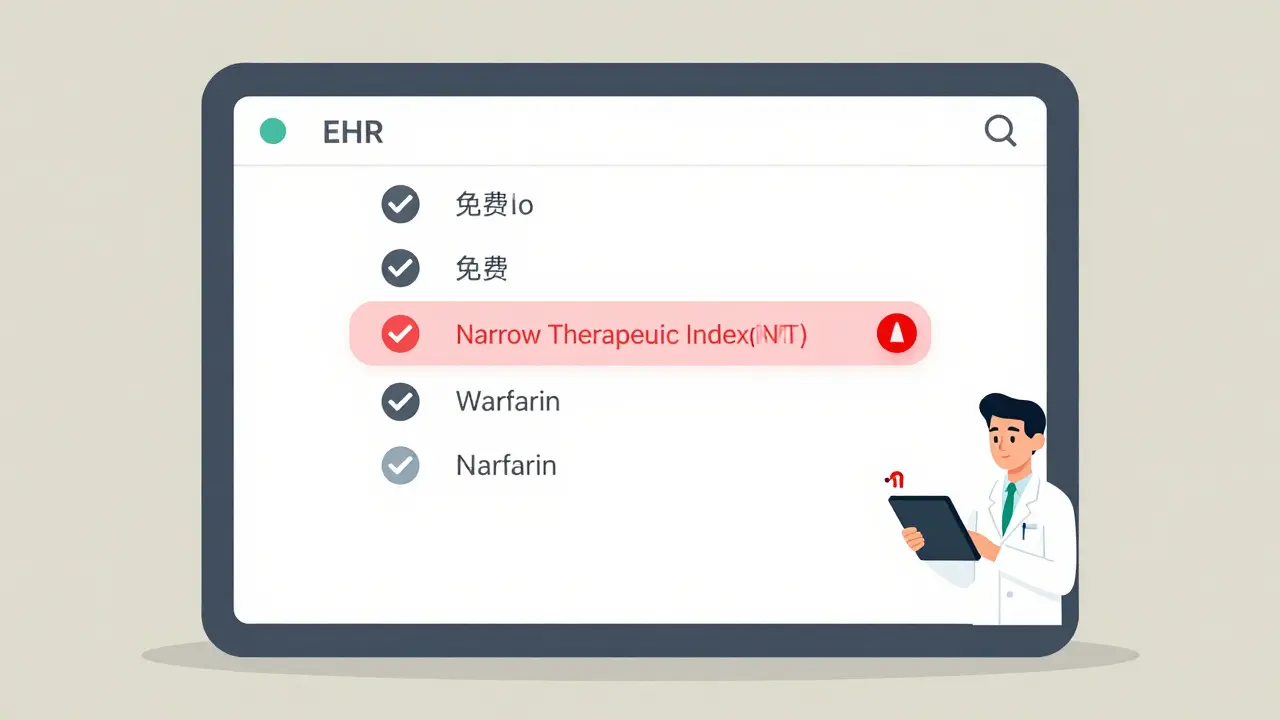
And it’s not just about consent. Some states treat Narrow Therapeutic Index (NTI) drugs differently. These are medications where even tiny changes in blood levels can cause harm - like warfarin, lithium, or phenytoin. Seventeen states require extra steps: physician notification, patient counseling, and sometimes even a second signature. Skip this, and you’re not just breaking policy - you’re risking patient safety.
What information must be documented? The non-negotiables
Regardless of state, there are five core pieces of information that must be captured every single time a substitution happens:
- The brand name prescribed
- The generic name dispensed
- The manufacturer of the generic drug
- The lot number
- The expiration date
Forty-eight states require all five. Missing one? Your pharmacy could face audit penalties, insurance claim denials, or worse - legal liability if something goes wrong. One 2021 case in the Journal of the American Pharmacists Association involved a warfarin substitution where the lot number wasn’t recorded. The patient later had a dangerous bleed. Without that data, no one could trace whether the issue came from the generic, the batch, or something else.
Time matters too. Forty-one states require documentation to be completed within 24 hours of dispensing. Delayed entries aren’t just sloppy - they’re risky. If a patient calls in panic two days later about a side effect, and the record isn’t there, you’ve lost your defense.
Electronic systems aren’t perfect - but they’re necessary
Most pharmacies now use digital systems to track substitutions. But not all systems are built the same. Epic Systems, one of the biggest EHR platforms, found in 2023 that 32% of pharmacies using their software had to customize their setup just to meet state documentation rules. That’s not a flaw in the software - it’s a flaw in the patchwork of state laws.
Pharmacists report spending an extra 20-30 seconds per prescription just to enter substitution details. That adds up. But the payoff? A 2022 study across 150 community pharmacies showed that full documentation cut medication errors by 17.3% in just six months. And according to the American Pharmacists Association, 23% of pharmacists say they’ve prevented an adverse event because they had the right records.
Chain pharmacies are ahead of the curve - 98% use electronic documentation. Independent pharmacies? 87%. That gap is shrinking. But the real win isn’t compliance. It’s safety.
What happens when documentation fails?
It’s not theoretical. In 2021, a patient in Florida was hospitalized after switching from one generic brand of levothyroxine to another. The pharmacist documented the substitution but didn’t note the manufacturer. The patient’s TSH levels went off the charts. Later, it turned out the new brand had a different filler that affected absorption. Had the lot number and manufacturer been recorded, the prescriber could have flagged it immediately. Instead, it took three weeks and a trip to the ER.
And it’s not just about mistakes. Insurance companies audit pharmacies constantly. If your records don’t show the substitution, they’ll deny payment. That means lost revenue - and potential investigations.
How to stay compliant in a changing landscape
Here’s what works:
- Know your state’s law - don’t assume it’s the same as your neighbor’s. Use the National Community Pharmacists Association’s online tool, updated quarterly.
- Train new staff for 4-6 weeks on documentation protocols. Don’t rush it.
- Use your pharmacy system’s alerts. Most modern systems can flag NTI drugs or missing fields before you dispense.
- When in doubt, document more. If you’re unsure whether consent was needed, get it. If you’re unsure whether the generic is equivalent, check the Orange Book.
- Keep a printed copy of your state’s substitution law on your desk. It’s not old-school - it’s smart.
The FDA says generics are safe. The WMA says substitutions for chronic conditions need doctor approval. The industry says documentation saves money. All of them are right. But only one thing matters in the moment: the patient in front of you.
What’s coming next?
The federal government is pushing for standardization. The Model State Pharmacy Act, updated in 2022, now recommends uniform documentation rules. Twelve states have already adopted them. The ASPE is drafting national guidelines expected in mid-2024. That could finally end the chaos.
Blockchain pilots are testing real-time, tamper-proof substitution logs. Early results show a 22% drop in documentation errors. That’s not sci-fi - it’s coming fast.
For now, though, you’re still working in a system of 50 different rules. The best defense? Consistency. Accuracy. And never skipping the record.
Documentation isn’t busywork - it’s your shield
Every time you document a substitution, you’re not just checking a box. You’re protecting a patient. You’re protecting your license. You’re protecting your pharmacy. The system isn’t perfect. The laws aren’t uniform. But your record? That can be flawless. And when it is, you’re not just following rules - you’re practicing better pharmacy.
Do I need patient consent to substitute a generic drug?
It depends on your state. In 27 states, pharmacists can substitute without consent. In 14 states, explicit patient consent is required. Nine states use a hybrid model. Always check your state’s pharmacy board rules. Some states, like Oklahoma, require written or verbal permission from either the prescriber or the patient before substitution.
What if I substitute a generic for a Narrow Therapeutic Index (NTI) drug?
Seventeen states have special rules for NTI drugs like warfarin, lithium, or levothyroxine. These require additional steps: physician notification, patient counseling, and often documentation of the manufacturer and lot number. Some states require a second signature. Never assume an NTI drug is safe to swap without checking your state’s specific protocols. The FDA doesn’t formally label NTI drugs in the Orange Book - so state law is your guide.
What happens if I forget to document a substitution?
Missing documentation can lead to insurance claim denials, pharmacy audits, fines, or even disciplinary action from your state board. In rare but serious cases, it can contribute to patient harm - like a medication error that goes undetected. Forty-one states require documentation within 24 hours. Delayed entries aren’t just risky - they’re violations.
Do I need to record the lot number and manufacturer every time?
Yes. Forty-eight states require the lot number and manufacturer name to be recorded for every generic substitution. This is critical for traceability in case of recalls or adverse events. One 2021 case linked a patient’s hospitalization to a specific lot of generic warfarin - because the lot number wasn’t documented, the cause couldn’t be confirmed.
Are electronic records enough, or do I need paper backups?
Electronic records are sufficient in all states, as long as they’re complete, secure, and accessible for audits. Paper backups are not required by law - but many pharmacies keep them for internal quality control. The key is that the electronic record must be reliable and meet your state’s technical requirements. Some states now require real-time electronic access for prescribers, like California’s SB 564.
Can a pharmacist refuse to substitute a generic even if it’s allowed?
Yes. Even in states where substitution is permitted without consent, pharmacists can choose not to substitute if they believe it’s not in the patient’s best interest. For example, if a patient has had a bad reaction to a specific generic manufacturer before, or if the drug is for a chronic condition and the prescriber has previously indicated no substitution. Always document your reason for refusing - it protects both you and the patient.
How often should I check my state’s substitution laws?
At least every quarter. Laws change - often. California updated its rules in January 2024. Other states have passed new laws in 2023 and 2024. Use the National Community Pharmacists Association’s online tool, which updates quarterly and cross-references state laws with documentation requirements. Don’t rely on memory or old training materials.




Yuri Hyuga
January 21, 2026 AT 02:10Coral Bosley
January 21, 2026 AT 06:09Steve Hesketh
January 23, 2026 AT 04:15Philip Williams
January 24, 2026 AT 07:30Ben McKibbin
January 25, 2026 AT 19:09Melanie Pearson
January 27, 2026 AT 12:29Rod Wheatley
January 29, 2026 AT 05:58Uju Megafu
January 30, 2026 AT 17:52Jarrod Flesch
January 31, 2026 AT 16:42Kelly McRainey Moore
February 1, 2026 AT 15:25Ashok Sakra
February 3, 2026 AT 09:46Gerard Jordan
February 3, 2026 AT 15:35michelle Brownsea
February 3, 2026 AT 17:40Roisin Kelly
February 5, 2026 AT 01:47Malvina Tomja
February 5, 2026 AT 18:44