
What drugs are actually hard to find right now?
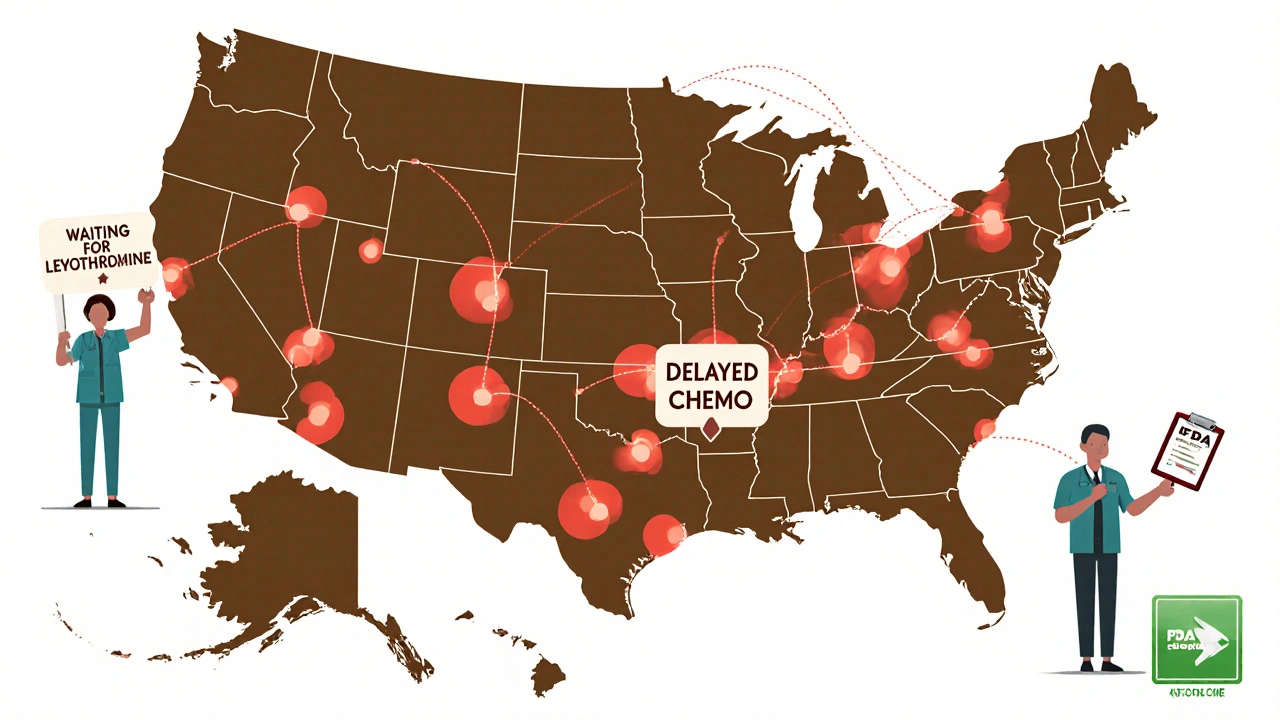
If you’ve been told your prescription is out of stock, or your hospital had to switch your treatment, you’re not alone. As of November 2025, more than 270 drugs are still in short supply across the U.S. - many for years. These aren’t rare specialty meds. They’re the ones doctors rely on every day: IV fluids, cancer drugs, antibiotics, and even basic glucose solutions used in emergency rooms and ICUs.
Why are these shortages still happening?
It’s not just bad luck. The problem runs deep. About 60% of the raw ingredients for U.S. medications come from just two countries: India and China. When a factory in India fails an FDA inspection - like the one that made half the country’s cisplatin - production stops. No backup. No quick fix. And because these are generic drugs, manufacturers barely make a profit. Why invest in more machines or better quality control when you’re selling a bag of saline for $1.50?
Meanwhile, demand keeps climbing. ADHD meds and weight-loss drugs like semaglutide have seen usage jump 35% a year since 2020. Factories can’t keep up. And when a single plant makes 70% of a drug, one shutdown can ripple across the country.
Which specific drugs are in short supply?
Some of the most critical shortages right now include:
- 5% Dextrose Injection (small bags) - Used for hydration, delivering meds, and treating low blood sugar. Shortage since February 2022, expected to last until August 2025.
- 50% Dextrose Injection - Critical for emergency hypoglycemia. Shortage since December 2021, not expected to resolve until September 2025.
- Cisplatin - A cornerstone chemotherapy drug for testicular, ovarian, and lung cancers. Still limited after a 2022 manufacturing failure in India.
- Vancomycin - A last-resort antibiotic for serious infections. In short supply since late 2024, forcing hospitals to ration doses.
- Levothyroxine - The main treatment for hypothyroidism. Shortages have returned in 2025 after a brief improvement in 2024.
- Procainamide - Used for abnormal heart rhythms. Only one U.S. manufacturer makes it, and production has been inconsistent.
These aren’t obscure drugs. They’re the backbone of emergency care, cancer treatment, and chronic disease management. A hospital pharmacist in Ohio told a Reddit thread how they had to prioritize cisplatin only for testicular cancer patients - because that’s where it works best. Other cancer patients got delayed or switched to less effective drugs.

Who’s affected the most?
It’s not just patients. Healthcare workers are drowning in the fallout.
Over 78% of doctors reported treatment delays in 2024 because they couldn’t get the right drug. Nearly half had to use alternatives that weren’t as effective or came with worse side effects. Pharmacists spend over 10 hours a week just tracking down meds or finding substitutions. And 67% say they’ve made medication errors because of last-minute switches - like giving the wrong dose or mixing up look-alike drugs.
For cancer patients, the numbers are worse. One in three experienced a treatment delay in 2024. On average, those delays lasted nearly two weeks. That’s not just inconvenience - it’s risk. For aggressive cancers, even a few days can change outcomes.
Why are generic drugs hit hardest?
Generic drugs make up 90% of prescriptions filled in the U.S. But they only bring in 20% of the industry’s revenue. That’s the problem.
Brand-name drugs have patents, higher prices, and bigger profit margins - often 30-40%. Generic makers? They fight over pennies. Margins are 5-8%. So when a factory needs a $10 million upgrade to meet FDA standards, the company often says: “Not worth it.”
And when demand spikes - like with weight-loss drugs - brand-name makers can raise prices and ramp up production. Generic makers? They’re stuck. No extra cash. No quick way to scale.
What’s being done to fix this?
The FDA says it stops about 200 potential shortages every year by stepping in early - warning manufacturers, helping them fix problems, or fast-tracking inspections. But they can’t force anyone to make more. No authority to demand production. No power to fine companies that sit on supplies.
Some states are trying their own fixes. New York is building an online map showing which pharmacies have which shortage drugs. Hawaii now lets Medicaid patients use foreign-approved versions of drugs if U.S. versions aren’t available. That’s smart - but it’s patchwork. We need a national system.
The U.S. Pharmacopeia wants three big changes: tax breaks for companies making raw ingredients in the U.S., mandatory stockpiles of critical drugs (like IV fluids and antibiotics), and a real-time national alert system that connects manufacturers, distributors, and hospitals. Right now, hospitals learn about shortages from other hospitals - not from official sources.
What can patients do?
If your medication is out of stock, don’t panic - but don’t wait either.
- Call your pharmacy before your refill is due. Ask if they have it in stock or when it’s expected.
- Ask your doctor if there’s a therapeutically equivalent alternative. For example, if 5% dextrose is out, sometimes 10% dextrose can be diluted safely - but only under medical supervision.
- Check the FDA’s Drug Shortages page (or ASHP’s database) for updates. Don’t rely on rumors.
- If you’re on a life-saving drug like cisplatin or levothyroxine, keep a 10-14 day supply on hand if possible. Talk to your doctor about backup plans.
Don’t switch meds on your own. Don’t skip doses. And don’t assume your doctor knows what’s available - many don’t. Bring the issue up early. Be persistent.
What’s next?
The Congressional Budget Office warns that without major policy changes, we’ll likely see over 250 shortages every year through 2027. If new tariffs on Chinese and Indian drug ingredients pass, that number could jump to 350.
We’ve known about this for years. We’ve had reports, hearings, and recommendations. But the system hasn’t changed. The same factories still make the same drugs. The same supply chains still snap under pressure. The same patients still wait.
This isn’t just a pharmacy problem. It’s a public health crisis. And until we treat it like one - with funding, accountability, and real planning - these shortages won’t go away. They’ll just get worse.
Why are IV fluids still in short supply in 2025?
IV fluids like 5% and 50% dextrose are still short because production is concentrated in just a few factories, most of them overseas. When one plant has a quality issue or shuts down for repairs, there’s no quick replacement. These are low-margin products, so manufacturers don’t invest in extra capacity. Demand has also increased as more patients are treated with IV hydration outside hospitals - in clinics and even at home.
Can I get my chemotherapy drug from another country?
In most cases, no. U.S. law requires all prescription drugs to meet FDA safety and quality standards. Even if a drug from Canada or India is chemically identical, it’s illegal to import it unless it’s approved by the FDA. Hawaii is the only state currently allowing foreign-approved versions under Medicaid during shortages - but that’s an exception, not the rule.
Are brand-name drugs also in short supply?
Yes, but less often. Brand-name drugs usually have higher profit margins, so manufacturers can afford to keep backup production lines or stockpile ingredients. Some brand-name drugs - especially newer ones like GLP-1 weight-loss medications - are actually in the worst shortages right now because demand has exploded faster than supply can grow.
Why don’t pharmacies just order more when they see a shortage coming?
They try - but the system doesn’t work that way. Drug distributors don’t stockpile. They deliver just-in-time to save money. Manufacturers don’t tell pharmacies when they’re running low - they tell the FDA. So pharmacies often find out about shortages the same time patients do: when the shelf is empty. Even if they wanted to buy extra, many can’t afford to tie up cash in inventory for drugs they might not sell for months.
How do I know if my medication is on the shortage list?
Check the FDA’s Drug Shortages page or the ASHP Drug Shortages Database. Both are updated weekly and list the drug name, manufacturer, reason for shortage, and expected resolution date. You can search by drug name or condition. Your pharmacist should also be able to check these for you - but don’t assume they know unless you ask.
Final thought: This isn’t going away quietly
Drug shortages aren’t temporary glitches. They’re structural failures. Until we rebuild the supply chain - with more domestic production, better transparency, and real financial incentives for manufacturers - we’ll keep seeing the same drugs disappear, the same patients delayed, and the same healthcare workers stretched thin.
It’s not about blame. It’s about action. And right now, that action is still missing.



Liam Strachan
November 20, 2025 AT 11:57Johannah Lavin
November 22, 2025 AT 06:57daniel lopez
November 23, 2025 AT 22:37Nosipho Mbambo
November 25, 2025 AT 15:48Michael Fessler
November 26, 2025 AT 09:56Ravinder Singh
November 27, 2025 AT 14:54Katie Magnus
November 28, 2025 AT 16:13Matthew Karrs
November 29, 2025 AT 01:03Dana Oralkhan
November 29, 2025 AT 19:28King Over
November 30, 2025 AT 11:14Destiny Annamaria
November 30, 2025 AT 18:35Ron and Gill Day
December 2, 2025 AT 06:45Gerald Cheruiyot
December 3, 2025 AT 00:39Russ Bergeman
December 3, 2025 AT 23:17Kristi Bennardo
December 4, 2025 AT 21:55