
When a doctor prescribes a generic medication, many assume it’s a simple step-fill the script, pick it up, done. But for providers across the U.S., that’s rarely the case. Even for low-cost generics, prior authorization often stands between the prescription and the patient’s hands. It’s not about stopping care-it’s about navigating a system designed to control costs, but one that’s increasingly slowing down care.
Why Generics Still Need Approval
You might think generics, being cheaper and just as effective, would fly through the system. But insurers don’t treat them that way. In fact, 28% of all prior authorization requests are for generic drugs, according to the Academy of Managed Care Pharmacy. Why? Because it’s not about the drug’s cost-it’s about control. Insurers and pharmacy benefit managers (PBMs) use prior authorization to steer patients toward specific versions of a generic. If there are five generic versions of lisinopril, the plan might only cover one made by a manufacturer they’ve negotiated a deeper discount with. Or maybe they’ve set a limit: only 30 tablets per month unless you prove you need more. Maybe the patient’s condition requires a longer course than the standard 8-week limit for proton pump inhibitors, and that needs documentation. It’s not random. These rules come from Pharmacy and Therapeutics (P&T) committees-teams of doctors and pharmacists who review clinical data and set guidelines. But the problem isn’t the guidelines. It’s how inconsistently they’re applied.The Step-by-Step Process
Securing approval for a generic isn’t one-size-fits-all. Here’s how it usually plays out:- Check the formulary. First, the provider or their staff looks up the patient’s insurance plan to see which generic versions are covered and under what conditions. Is there a preferred brand? Are there quantity or duration limits?
- Document the medical necessity. This is where it gets real. If the patient had an allergic reaction to the preferred generic, or if they tried three other generics and none worked, that needs to be in writing. Lab results, clinic notes, diagnostic reports-all of it matters. Pennsylvania’s Department of Human Services explicitly says: no approval without chart notes or test results.
- Submit electronically. Over 78% of commercial insurers and 63% of Medicare Part D plans now require electronic submission through systems like CoverMyMeds or Surescripts. Fax is fading. Phone requests? Rare. The faster you go digital, the faster you get a response.
- Wait for a decision. Medicaid must respond in 24 hours for urgent cases and 14 days for routine ones. Commercial insurers? Typically 5-10 business days. But if the paperwork is incomplete? That clock resets.
- Get approved-or denied. If approved, the pharmacy gets the green light. If denied, the provider must appeal or switch meds. About 18.7% of generic prior auth requests get denied, mostly because of missing documentation or not proving medical necessity.
What Makes Approval Faster for Generics?
Here’s the silver lining: generic prior authorizations are often approved quicker than brand-name ones. Why? Because insurers know generics are interchangeable. There’s less risk. If a patient needs omeprazole 40mg daily and the plan allows 30 tablets, and the patient has a history of taking it without issue? Auto-approval kicks in. Judi Health reports that 41% of generic prior auth requests are auto-approved when quantity limits aren’t exceeded and the patient’s history matches the criteria. Express Scripts saw a 40% jump in auto-approvals for generics in 2023. That’s because the system is learning. AI-assisted tools are now scanning claims history, checking formulary rules, and flagging low-risk requests-no human needed. But here’s the catch: auto-approval only works if the data is clean. If the patient’s allergy to one generic isn’t documented in the system, or if the prescribing provider used a different name for the drug (like “Prilosec” instead of “omeprazole”), the system flags it as uncertain. That’s when it goes to a human-and delays start piling up.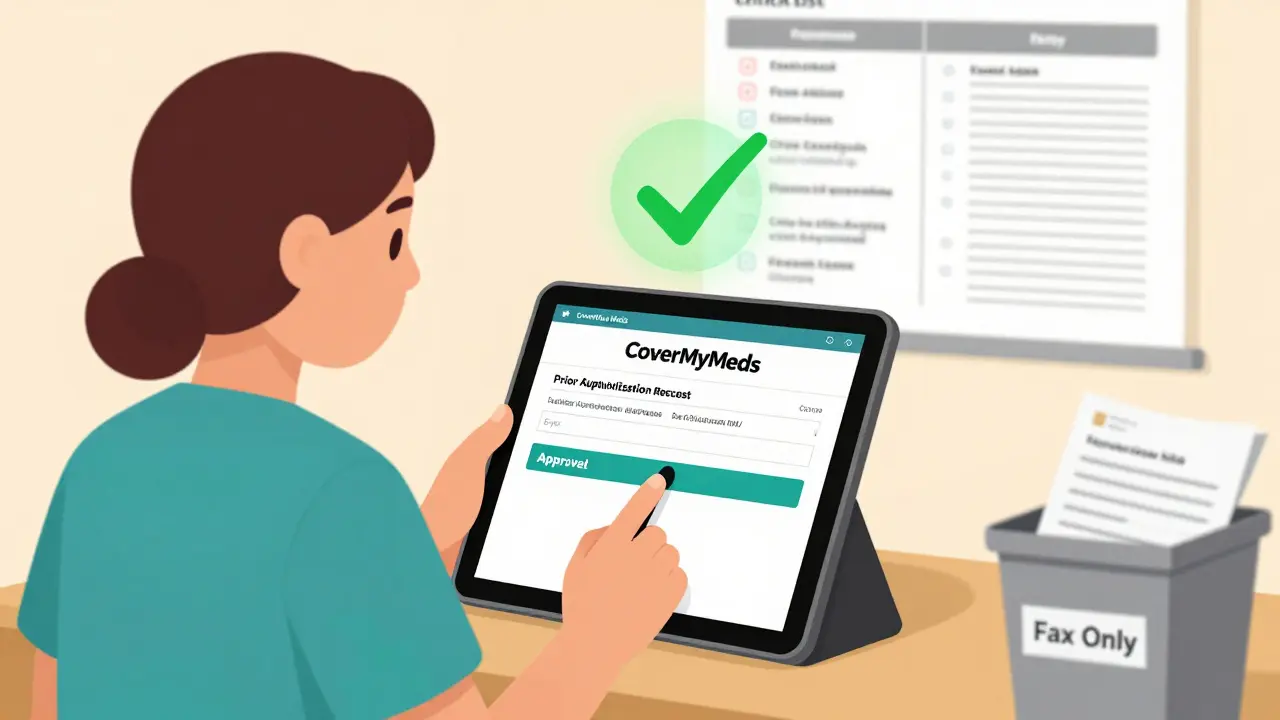
Real Stories from the Front Lines
Dr. Michael Chen on Reddit shared how he got approval for omeprazole 40mg daily for 12 weeks for a patient with Barrett’s esophagus. He attached the endoscopy report showing intestinal metaplasia. Submitted via CoverMyMeds. Approved in two business days. Then there’s Dr. Lisa Rodriguez on Sermo. She prescribed generic sitagliptin after a patient couldn’t tolerate metformin. The insurer denied it-demanding proof the patient tried three other diabetes drugs first. But the American Diabetes Association guidelines say metformin intolerance alone is enough to switch. The insurer didn’t care. It took three weeks and two appeals to get it approved. These aren’t outliers. They’re everyday experiences. A 2023 survey by the National Community Pharmacists Association found that 83% of pharmacists have had patients walk out because they couldn’t afford to pay cash for a generic while waiting for approval. That’s not just inconvenient. It’s dangerous.How Providers Are Fighting Back
Providers aren’t just sitting back. They’re building systems to win this game. - Dedicated staff. Medical assistants now handle 78% of routine prior auth requests under physician supervision. Training takes 2-3 weeks, but it saves doctors 16 hours a week-time they’d otherwise spend on paperwork instead of patients. - Templates. Standardized documentation templates for common scenarios (like PPIs, statins, or diabetes meds) cut approval times by 32%, according to Capital Rx. - Payer-specific checklists. Every insurer has different rules. One might need a letter of medical necessity. Another might require a prior prescription history. Providers who keep these in a digital folder save hours. - Automated tracking. Tools that alert staff when a request hasn’t been answered in five days. No more “Did they get it?” phone calls. The American Medical Association recommends all practices do this. But only 40% of small practices have a dedicated prior auth team. The rest? They’re drowning in faxes and portal logins.
The Bigger Picture: Costs, Reform, and the Future
Prior authorization saves money-$4.2 billion a year on generic misuse alone, according to CMS. But it also costs the system. The Congressional Budget Office estimates providers will spend $1.2 billion more on administrative work by 2026 if nothing changes. New rules are coming. As of January 1, 2024, Medicare Advantage plans must respond to 90% of prior auth requests within 72 hours for standard cases. In July 2024, Medicaid managed care plans had to switch to standardized electronic transactions-cutting processing times by an estimated 25%. The AMA is pushing state laws to eliminate prior authorization for generics that have been on the market for more than five years and have multiple manufacturers. That’s smart. If there are 15 versions of metformin, why does the insurer get to pick which one you get? By 2026, McKinsey predicts 75% of generic prior auth decisions will be made by AI systems. That could mean approvals in under 24 hours. But only if the data feeding those systems is accurate-and if the rules aren’t designed to block care in the first place.What Patients Need to Know
Patients don’t control this system. But they can help. If your doctor says you need prior authorization:- Ask: “Is there a generic version that doesn’t need approval?”
- Ask: “Can you send the paperwork electronically?”
- Ask: “How long will this take?”
- If you can’t afford to pay out of pocket while waiting, tell your pharmacist. Some pharmacies have short-term assistance programs.
What’s Next for Providers
The future belongs to those who automate, standardize, and document. Practices that invest in electronic systems, train staff, and build relationships with payer reps are seeing approval rates climb. Those still relying on paper and phone calls? They’re falling behind. The goal isn’t to eliminate prior authorization. It’s to make it work for patients-not against them. For generics, that means fewer hoops, clearer rules, and faster decisions. And with AI and new regulations on the horizon, change is coming. The question is: will providers be ready?Why do insurance companies require prior authorization for generic drugs?
Insurers require prior authorization for generics to control costs and steer patients toward specific versions they’ve negotiated lower prices for. Even though generics are cheaper than brand-name drugs, insurers may limit which manufacturer’s version they cover, set quantity or duration limits, or require proof that other generics failed. This helps them manage formulary spending, but it often adds unnecessary steps for patients and providers.
How long does prior authorization for generics usually take?
For generics, approval typically takes 1-3 business days when documentation is complete and submitted electronically. Medicaid must respond within 24 hours for urgent cases and 14 days for standard ones. Commercial insurers usually take 5-10 business days. If paperwork is missing, the clock resets, and delays can stretch to 7-14 days. Auto-approval systems can approve some requests in minutes if the patient’s history matches the plan’s rules.
What documents are needed to get prior authorization for a generic?
Providers need to submit clinical documentation proving medical necessity. This includes clinic notes, lab results, diagnostic reports (like endoscopies or MRIs), and records showing prior medication failures or adverse reactions. For example, if a patient had a rash on one generic version of lisinopril, that reaction must be clearly documented. Some insurers also require a letter explaining why the requested generic is needed over the preferred one.
Can prior authorization be denied for a generic even if it’s medically necessary?
Yes. Denials happen even when the drug is medically necessary. Common reasons include missing documentation (42% of denials), failure to prove the patient tried a preferred alternative (20%), or the insurer’s formulary rules not matching clinical guidelines (38%). For instance, a patient may have intolerance to metformin, but the insurer still demands proof they tried two other diabetes drugs first-even though guidelines say that’s unnecessary.
Are there any new laws making prior authorization easier for generics?
Yes. The Improving Seniors’ Timely Access to Care Act of 2023 requires Medicare Advantage plans to respond to 90% of prior authorization requests within 72 hours for standard cases, effective January 2024. Medicaid managed care plans must now use standardized electronic transactions, cutting processing times by 25% as of July 2024. The AMA is also pushing state laws to eliminate prior authorization for generics that have been on the market for over five years with multiple manufacturers.
What can providers do to speed up prior authorization for generics?
Providers can speed up approvals by using electronic submission systems like CoverMyMeds, maintaining standardized documentation templates for common scenarios, training staff to handle routine requests, and keeping payer-specific checklists. Practices with dedicated prior auth teams see approval times drop by 32%. Auto-approval pathways are also more likely to trigger when documentation is consistent and complete.
Do all insurance plans require prior authorization for generics?
No, but most do. As of 2024, 93% of commercial insurance plans, 89% of Medicare Part D plans, and 67% of Medicaid fee-for-service programs require prior authorization for at least some generic medications. Plans with strict formularies and PBM contracts are the most likely to impose restrictions, especially for drugs with multiple generic options.
What happens if a patient can’t afford the generic while waiting for approval?
Many patients skip doses or go without medication entirely. A 2023 survey found that 83% of pharmacists have seen patients unable to pay out-of-pocket for a generic while waiting for approval. Some pharmacies offer short-term assistance programs, and manufacturers sometimes provide free samples. Providers can also request an emergency override or bridge prescription if the condition is urgent.



Urvi Patel
January 1, 2026 AT 12:07This is why American healthcare is a joke. You're telling me a $5 pill needs a PhD-level bureaucracy to get approved? I've seen more efficient customs clearance in Mumbai. This isn't healthcare-it's a corporate obstacle course designed to make providers beg for pennies.
And don't even get me started on the 'auto-approval' myth. If your system can't recognize 'lisinopril' as the same drug across 15 manufacturers, it's not AI-it's a glitchy Excel sheet with a fancy name.
anggit marga
January 1, 2026 AT 19:28Who even cares? In Nigeria we just walk into a pharmacy and buy what the doctor says. No forms. No fax. No waiting. Why are Americans so obsessed with paperwork? You have the technology to auto-approve in minutes but you choose to make doctors into clerks? This isn't innovation-it's colonial thinking with a US flag.
Stop pretending this is about cost control. It's about profit. Plain and simple.
Joy Nickles
January 1, 2026 AT 23:59Okay but like… why is everyone acting surprised? This is EXACTLY what happens when you outsource healthcare decisions to PBMs who don’t even have MDs. I work in health tech and I’ve seen the internal dashboards-90% of prior auth denials are because the system can’t parse ‘Prilosec’ vs ‘omeprazole’ or someone forgot to check the ‘box’ for ‘previous trial failed’.
And don’t get me started on the ‘standardized templates’-they’re just copy-paste garbage that makes the AI worse. Also, why is everyone ignoring that 42% of denials are due to missing documentation? That’s not a system failure-that’s a training failure. And guess who pays? The patient. Again.
Also-why are we still talking about faxes in 2024???
Emma Hooper
January 2, 2026 AT 09:47Oh honey. This isn’t broken-it’s *designed* this way. Insurance companies aren’t evil geniuses. They’re just lazy accountants who got promoted because they could spell ‘formulary’ without Google. They don’t care if your grandma’s blood pressure spikes because she waited three weeks for a $5 pill. They care about the quarterly report.
But here’s the silver lining: the system’s finally cracking. AI is learning. Providers are fighting back with templates and dedicated staff. And patients? They’re getting smarter. They’re asking ‘Can you send this electronically?’-and that’s the real revolution.
It’s not pretty. It’s not fair. But it’s changing. Slowly. Like a snail on caffeine.
And yes-I’ve had my own prior auth nightmare with metformin. Took 17 days. I cried. Then I emailed my senator. And you should too.
Martin Viau
January 3, 2026 AT 10:07Let’s be clear: prior authorization for generics is a regulatory arbitrage play. PBMs use formulary restrictions to extract rebates from manufacturers, shifting cost burdens downstream to providers and patients. The clinical utility of the drug is irrelevant-the economic incentive structure is the only variable that matters.
AI-driven auto-approval is a band-aid. What we need is structural reform: eliminate PBM rebate secrecy, mandate formulary transparency, and decouple drug pricing from administrative gatekeeping. Until then, we’re just rearranging deck chairs on the Titanic.
Also-why are we still using CoverMyMeds? It’s 2024. We have HL7 FHIR. We have blockchain. We have AI. And we’re still faxing lab reports? Pathetic.
Robb Rice
January 4, 2026 AT 10:26It’s frustrating, but the system isn’t entirely without logic. Prior auth does prevent overuse and misuse-even for generics. I’ve seen patients on 120mg of omeprazole daily because they didn’t understand their diagnosis. The system catches that.
That said, the execution is a disaster. The lack of interoperability between EHRs and payer systems is criminal. And the fact that a single typo in drug name can derail a 3-week approval? That’s not efficiency-that’s negligence.
Providers need better training, better tools, and more accountability from payers. And patients? They need to know their rights. This isn’t about blame. It’s about fixing what’s broken.
Harriet Hollingsworth
January 4, 2026 AT 20:57Someone needs to go to jail for this. I mean, really. A 40-year-old with high blood pressure waits two weeks for a $5 pill because someone didn’t fill out a form right? That’s not a healthcare failure. That’s a moral failure. That’s cruelty dressed up as policy.
And don’t give me that ‘it saves money’ crap. You’re saving pennies while costing lives. People die waiting for meds. I’ve seen it. My cousin died because she skipped her insulin while waiting for prior auth. And now you’re all here talking about AI and templates like it’s a TED Talk?
Stop pretending this is complicated. It’s not. It’s evil. And you’re all complicit.
Deepika D
January 6, 2026 AT 20:22Hey everyone-just wanted to share what’s working in my clinic. We started training our medical assistants to handle prior auths with a simple 3-step checklist: 1) Check formulary on our internal database (we built it ourselves), 2) Use our pre-written template for common meds like statins and PPIs, 3) Submit via CoverMyMeds with a checklist of required docs attached.
It sounds boring, but it cut our approval time from 8 days to 2.5 days. We also started keeping a folder for each insurer’s weird rules-like how Blue Cross wants a letter signed by the MD, but UnitedHealthcare just needs a checkbox. We printed them out and laminated them. Yes, really.
And here’s the thing: we didn’t need fancy AI. We just needed to stop treating this like a puzzle and start treating it like a process. Anyone can do this. You don’t need a PhD. You just need to be organized.
If you’re a small practice drowning in faxes, I’ll send you our template. No charge. Just pay it forward when you can.
Also-patients, if your doctor says ‘we’re submitting it,’ don’t wait. Call the pharmacy. Ask if they’ve received the e-request. Most don’t even know to ask. You’re your own best advocate.
We’re not perfect. But we’re trying. And that’s more than most.