One in three American adults is at risk for kidney disease - and most don’t even know it. Kidney disease prevention isn’t just about avoiding illness; it’s about stopping something silent before it steals your health. The kidneys filter waste, balance fluids, and regulate blood pressure. When they fail, the body pays a heavy price: $128 billion a year in Medicare costs, and 300,000 preventable cases of kidney failure each year. The good news? You don’t need a miracle. You need to change a few daily habits.
What Actually Causes Kidney Disease?
Most cases of chronic kidney disease (CKD) aren’t random. They’re the result of long-term damage from conditions you can control. Diabetes and high blood pressure are the big two, responsible for nearly 75% of all cases. If your blood sugar stays high for years, it slowly scars the tiny filters in your kidneys. High blood pressure does the same thing - it crushes those delicate vessels until they can’t do their job anymore. But it doesn’t stop there. Obesity, smoking, and long-term use of over-the-counter painkillers like ibuprofen or naproxen also chip away at kidney function. People who take NSAIDs daily for headaches or back pain are at higher risk - these drugs reduce blood flow to the kidneys, and over time, that leads to damage. And if you’ve got a family history of kidney disease, your risk goes up even more. Here’s the scary part: CKD has no symptoms in the early stages. You won’t feel tired, you won’t have pain, and you won’t notice swelling. By the time symptoms show up, the damage is often advanced. That’s why knowing your risk factors is the first step to protecting yourself.How Much Salt Are You Really Eating?
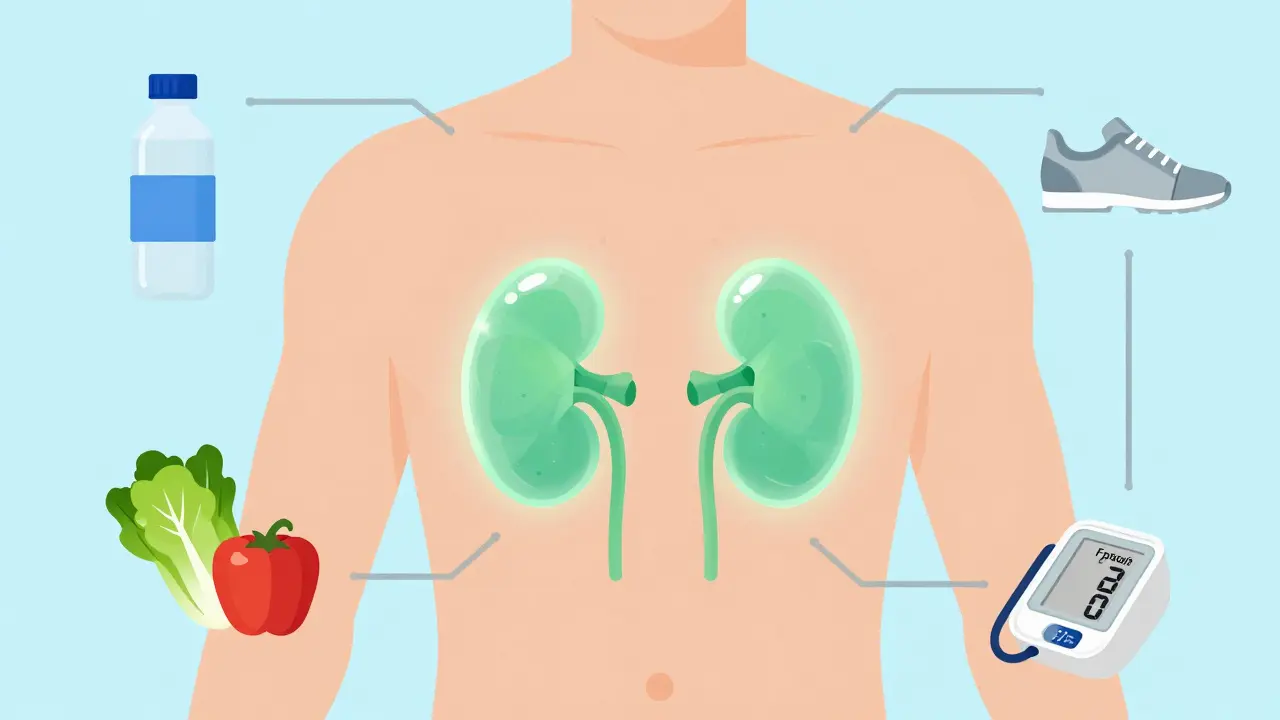
Sodium isn’t just about salty snacks. It’s in bread, canned soup, deli meats, sauces, and even breakfast cereal. The average American eats over 3,400 mg of sodium a day. The target for kidney health? Under 2,300 mg - that’s about one teaspoon of salt. Cutting sodium doesn’t mean giving up flavor. It means reading labels. Choose fresh or frozen vegetables instead of canned. Cook at home more often. Use herbs, lemon juice, garlic, and vinegar to season food instead of salt. If you’re eating out, ask for sauces on the side and skip the extra salt. Why does this matter? High sodium intake raises blood pressure. And high blood pressure is the number one driver of kidney damage. For someone with diabetes or pre-hypertension, reducing salt can slow kidney decline by up to 40% in early stages.Move More - It’s Not About Running Marathons
You don’t need to hit the gym five days a week. The CDC and NHS agree: 150 minutes of moderate activity per week is enough. That’s 30 minutes, five days a week. Walk after dinner. Take the stairs. Dance while cooking. Ride a bike to the store. Exercise helps in three big ways: it lowers blood pressure, helps control blood sugar, and reduces body fat. All three protect your kidneys. A 2022 study from the American Kidney Fund showed that people who started walking 30 minutes a day reduced their risk of kidney decline by 25% over two years - even without losing weight. Strength training matters too. Two days a week of lifting weights, using resistance bands, or doing bodyweight exercises like squats and push-ups helps your body use insulin better. That’s critical if you have prediabetes or type 2 diabetes.What You Eat Matters More Than You Think
A kidney-friendly diet isn’t a special “kidney diet.” It’s just a healthy one. The NHS recommends five portions of fruits and vegetables daily, whole grains, lean proteins, and low-fat dairy. Avoid processed foods. Limit saturated fats. Cut out sugary drinks. Sugar is a silent killer for kidneys. A single 12-ounce soda can contain 40 grams of sugar - that’s 10 teaspoons. The CDC says sugary drinks make up 7% of the average American’s daily calories. That sugar doesn’t just cause weight gain - it spikes insulin, inflames blood vessels, and damages the kidneys over time. Protein intake needs balance too. Too much - especially from red meat or processed meats - can overload the kidneys. Aim for lean sources: chicken, fish, beans, tofu. The general rule: don’t eat more than 0.8 to 1.2 grams of protein per kilogram of body weight. For a 150-pound person, that’s about 55-80 grams a day.
Stop Smoking - Your Kidneys Will Thank You
Smoking doesn’t just hurt your lungs. It narrows the blood vessels that feed your kidneys. Smokers have a 50% higher risk of kidney function decline than non-smokers. If you already have kidney disease, smoking makes it progress 30-50% faster. Quitting isn’t easy, but it’s the single most effective thing you can do for your kidneys after controlling blood pressure and blood sugar. Within two years of quitting, kidney damage slows down significantly. And within five years, your risk of kidney failure drops close to that of someone who never smoked.Alcohol, Medications, and What to Avoid
One drink a day for women, two for men - that’s the limit. More than that, and you’re increasing your risk of high blood pressure and liver damage, both of which strain the kidneys. Alcohol also dehydrates you, which makes your kidneys work harder. Painkillers like ibuprofen, naproxen, and aspirin are dangerous if taken daily. They’re not harmless. The FDA estimates that 3-5% of new kidney disease cases each year come from overuse of these drugs. If you need pain relief regularly, talk to your doctor about safer options like acetaminophen - and never take NSAIDs without medical advice if you have high blood pressure, diabetes, or existing kidney issues. Also, get your flu shot every year. People with kidney disease are 3-5 times more likely to end up in the hospital from the flu. Vaccination isn’t optional - it’s essential.Check Your Numbers - Regularly
If you have diabetes, get your A1C tested at least twice a year. Aim for under 7% - but talk to your doctor about your personal goal. For blood pressure, the target is 120/80 mm Hg. If you’re over 40, or have diabetes, high blood pressure, or a family history of kidney disease, get tested annually. Two simple tests can catch kidney disease early: a blood test for creatinine (which calculates your GFR) and a urine test for albumin. If your GFR is below 60 for three months, or if albumin is in your urine, you may have early kidney damage. Catching it now means you can stop it from getting worse.Weight Loss Isn’t Just About Looks
Losing just 5 kg (about 11 pounds) reduces your risk of kidney disease by 25-30%. That’s not a guess - it’s from the National Kidney Foundation’s 2023 guidelines. Every pound lost lowers blood pressure, improves insulin sensitivity, and reduces inflammation. You don’t need to lose 50 pounds. Start with 5. Walk 10 minutes after each meal. Swap soda for water. Eat one less processed snack a day. Small steps add up.Stress and Sleep - The Hidden Factors
Chronic stress raises cortisol, which increases blood pressure and blood sugar. A Johns Hopkins study found that people who practiced mindfulness or meditation for 10-15 minutes a day had 15% slower kidney function decline over three years. Sleep matters too. Poor sleep disrupts hormones that regulate blood pressure and metabolism. Aim for 7-8 hours a night. If you snore or wake up tired, get checked for sleep apnea - it’s strongly linked to both high blood pressure and kidney disease.Who Needs to Be Extra Careful?
Black Americans are 3.4 times more likely to develop kidney failure than White Americans. Hispanic Americans are 1.3 times more likely. Why? Higher rates of diabetes and hypertension, plus less access to early screening and care. If you’re from one of these groups, or if you have a family history of kidney disease, diabetes, or high blood pressure, don’t wait for symptoms. Get tested now. Talk to your doctor about a prevention plan.What’s Working Right Now?
Telehealth is making prevention easier. A 2021 pilot study showed that patients using remote blood pressure monitors had 37% better medication adherence. Apps that track food, water, and activity are helping people stick to their goals. The CDC’s new “Get Ahead of CKD” campaign is pushing for free screening in community clinics. And new research is identifying genetic markers that predict who’s most at risk - so prevention can be personalized.Start Today - Not Tomorrow
You can’t change your genes. But you can change your plate, your steps, your sleep, your smoke, your salt. Kidney disease isn’t inevitable. It’s often preventable - if you act before it’s too late. The next time you reach for a soda, a bag of chips, or a painkiller, pause. Ask yourself: Is this helping my kidneys - or hurting them? Your kidneys don’t ask for much. Just a little care, every day.Can kidney disease be reversed?
Early-stage kidney damage (Stages 1-2) can often be slowed or even reversed with lifestyle changes like lowering blood pressure, controlling blood sugar, reducing salt, and losing weight. Once scarring sets in (Stage 3 and beyond), the damage is permanent - but further decline can still be prevented with the right care.
What foods should I avoid if I want to protect my kidneys?
Avoid processed foods, canned soups, deli meats, salty snacks, sugary drinks, and foods high in saturated fat. Limit red meat and full-fat dairy. Choose fresh fruits, vegetables, whole grains, lean proteins like fish and chicken, and unsalted nuts instead.
How much water should I drink for kidney health?
There’s no one-size-fits-all number. Drink enough so your urine is light yellow - about 6-8 cups a day for most people. If you’re active, live in a hot climate, or have diabetes, you may need more. Don’t overdo it - drinking too much water won’t give you extra kidney protection.
Is it safe to take ibuprofen if I have high blood pressure?
No. Ibuprofen and other NSAIDs can reduce blood flow to the kidneys and raise blood pressure. If you have high blood pressure, diabetes, or any kidney risk, talk to your doctor before using these medications. Acetaminophen is usually safer for occasional use.
Can I prevent kidney disease if it runs in my family?
Yes. Genetics increase your risk, but they don’t determine your fate. People with a family history of kidney disease can reduce their risk by 50% or more by controlling blood pressure, staying at a healthy weight, avoiding smoking, and getting regular screenings.
How often should I get my kidneys checked?
If you have diabetes, high blood pressure, obesity, or a family history of kidney disease, get tested every year. The tests are simple: a blood test for creatinine and a urine test for albumin. If you’re healthy and under 40 with no risk factors, testing every 3-5 years is fine.
Does drinking cranberry juice help kidney health?
Cranberry juice may help prevent urinary tract infections, but it doesn’t protect your kidneys from diabetes or high blood pressure damage. Many commercial juices are loaded with sugar, which harms your kidneys. Stick to water and unsweetened drinks.
Can losing weight improve kidney function?
Yes. Losing just 5-10% of your body weight can lower blood pressure, improve insulin sensitivity, and reduce protein in the urine - all signs that your kidneys are under less stress. Weight loss is one of the most effective ways to protect kidney function.



Aurelie L.
January 27, 2026 AT 01:17I used to eat canned soup every day. Then my dad had a stroke. Now I cook everything from scratch. No more hidden salt.
It’s not hard. Just read the label.
That’s it.
Joanna Domżalska
January 28, 2026 AT 02:00Everyone says 'control blood pressure' like it's a button you press. What if your job is 12-hour shifts and you’re on food stamps? You think your kidneys care about your hustle?
Stop blaming people for being poor. The system broke their kidneys first.
Faisal Mohamed
January 29, 2026 AT 18:25Bro, the nephrotoxic cascade induced by chronic NSAID exposure is a silent epidemic masked by wellness culture. 🤔
We’re optimizing for dopamine, not glomerular filtration rate. 🧠💧
Also, hydration isn’t about volume-it’s about osmotic homeostasis. 🌊✨
Josh josh
January 31, 2026 AT 17:49just stop eating chips and soda and youll be fine
no need for all this fancy stuff
my grandma lived to 92 and never checked a single number
she drank coke and smoked
so maybe the whole thing is fake
bella nash
February 2, 2026 AT 03:29It is imperative to underscore that the etiology of chronic kidney disease is multifactorial, and behavioral modification alone cannot supersede the necessity of systemic healthcare intervention.
Individual responsibility, while commendable, is insufficient in the context of structural inequities in renal care access.
Moreover, the conflation of dietary compliance with moral virtue is both scientifically inaccurate and ethically problematic.
Sally Dalton
February 2, 2026 AT 11:40omg i just realized i’ve been eating canned tuna every day for years 😭
i’m gonna start cooking tonight!!
and i’m gonna drink water instead of diet coke!!
and walk after dinner!!
thank you for this post!!
you made me feel like i can actually do something good for myself 💕
even if i mess up tomorrow, today i tried!!
Shawn Raja
February 3, 2026 AT 01:40Wow. So the solution to kidney failure is… not being lazy? And not being broke? And not being Black?
Real deep stuff here.
Meanwhile, the guy who works two jobs and eats gas station food because his town has no grocery store? He’s just not trying hard enough?
Real compassionate. 🤡
Ryan W
February 3, 2026 AT 21:49Let’s be real. This article reads like a pharmaceutical ad disguised as public health advice.
NSAIDs are fine if you’re not diabetic. Stop fearmongering.
And why is everyone suddenly obsessed with sodium? My grandpa ate 5 tablespoons of salt daily and lived to 98.
Also, the CDC is full of woke bureaucrats who think salt is a hate crime.
Stop overmedicalizing normal life.
Allie Lehto
February 5, 2026 AT 15:34you know what? i had stage 2 kidney damage last year.
i stopped soda.
i walked 20 mins every night.
i cooked my own food.
i quit smoking.
i lost 15 lbs.
my GFR went from 58 to 76 in 8 months.
no meds. no surgery. just me.
if i can do it, you can too.
your kidneys are listening.
stop ignoring them.
please.
❤️