
What Is Polycystic Ovary Syndrome (PCOS)?
Polycystic Ovary Syndrome, or PCOS, isn’t just about cysts on the ovaries. It’s a hormonal disorder that affects 5 to 10% of women during their reproductive years. You might hear it called a "polycystic ovary," but the real issue isn’t the cysts-it’s the chaos in your hormones. Three main signs define PCOS: irregular or missing periods, too many male hormones (like testosterone), and ovaries that look swollen with small follicles on ultrasound. You only need two of these three to get diagnosed, according to the Rotterdam criteria used worldwide since 2003.
Many women don’t realize they have PCOS until they try to get pregnant. That’s because symptoms like acne, extra body hair, or weight gain often get brushed off as normal teenage issues or stress. On average, it takes 2 to 3 years after symptoms start before someone gets a proper diagnosis. And it’s not just about fertility. PCOS is tied to insulin resistance in 50 to 70% of cases, even in women who aren’t overweight. That means your body struggles to use insulin properly, which pushes your ovaries to make more testosterone and messes with your menstrual cycle.
The Hormonal Imbalance Behind PCOS
The core problem in PCOS is a tangled web of hormones working against each other. Testosterone, the main male hormone, is often 1.5 to 2 times higher than normal in women with PCOS. That’s why so many deal with unwanted facial or chest hair (hirsutism), stubborn acne, or thinning hair on the scalp. But testosterone doesn’t act alone. High insulin levels-caused by insulin resistance-tell your ovaries to make even more of it. At the same time, your liver produces less sex hormone-binding globulin (SHBG), which normally keeps testosterone in check. So your body ends up with more free, active testosterone floating around.
Your brain’s signaling system is also off. Luteinizing hormone (LH), which tells your ovaries to release an egg, is often too high-sometimes more than double the level of follicle-stimulating hormone (FSH). This imbalance prevents follicles from maturing properly. Instead of one dominant egg being released each month, you get a bunch of tiny, stuck follicles. That’s what shows up on an ultrasound as "polycystic" ovaries. Without ovulation, progesterone doesn’t rise. That leaves estrogen unopposed, which can lead to thickened uterine lining and, over time, raise the risk of endometrial cancer.
Stress makes it worse. When cortisol spikes from chronic stress, it throws off the hypothalamic-pituitary-ovarian axis-the brain’s control center for reproduction. Even small amounts of extra stress can delay or stop ovulation in women with PCOS. And it’s not just hormones. Studies show that 30 to 50% of women with PCOS also struggle with depression or anxiety, which often goes untreated because doctors focus only on fertility or skin issues.
Fertility Treatment: Where to Start
If you’re trying to get pregnant and have PCOS, the first step isn’t medication-it’s lifestyle. Losing just 5 to 10% of your body weight can restore ovulation in 30 to 50% of overweight women. That doesn’t mean starving yourself. It means moving more and eating smarter. The Diabetes Prevention Program model works well: 150 minutes of moderate exercise per week (like brisk walking) and cutting 500 to 750 calories daily. Studies show this brings back regular periods in 44% of women who hadn’t ovulated in months.
Once lifestyle changes are in place, doctors turn to ovulation-inducing drugs. Clomiphene citrate (Clomid) has been the go-to for decades. It works by tricking your brain into releasing more FSH. About 60 to 85% of women ovulate on Clomid, and 30 to 40% get pregnant within six cycles. But it’s not perfect. Around 20 to 25% of women don’t respond at all. That’s where letrozole comes in. Originally a breast cancer drug, letrozole is now the preferred first-line treatment for PCOS infertility. In the landmark PPCOS-II trial, women on letrozole had higher ovulation rates (88% vs. 70%) and better live birth rates (27.5% vs. 19.1%) than those on Clomid. It’s now recommended as the first choice by major guidelines in the U.S. and Europe.
When Medications Don’t Work: Next Steps
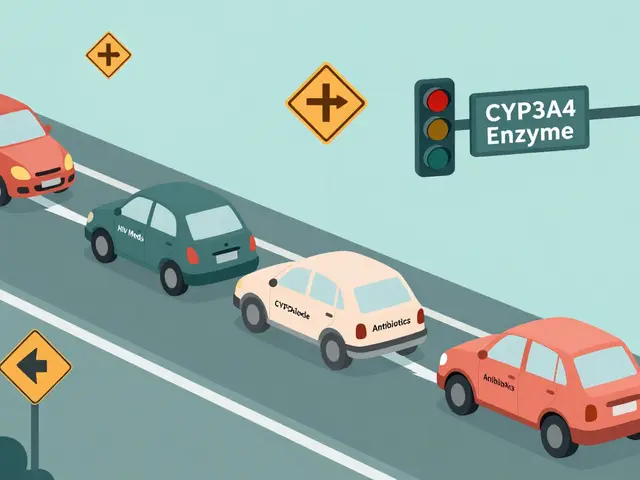
If letrozole doesn’t lead to pregnancy after three to six cycles, your doctor might suggest metformin. This diabetes drug improves insulin sensitivity and can help restart ovulation, especially in women with high insulin levels or a BMI over 35. But metformin alone isn’t strong enough for most people. It works best when combined with Clomid or letrozole-boosting pregnancy rates by 30 to 50% compared to either drug alone. The catch? About half of people stop taking it within six months because of stomach upset: nausea, bloating, or diarrhea. Starting with a low dose and increasing slowly helps a lot.
If oral medications fail, the next step is injectable gonadotropins. These are pure FSH and LH hormones that directly stimulate the ovaries. They’re more powerful but also riskier. About 20 to 30% of women on gonadotropins end up pregnant per cycle, but the chance of twins or triplets jumps to 20 to 30%. There’s also a 5 to 10% risk of ovarian hyperstimulation syndrome (OHSS), where ovaries swell and fluid leaks into the abdomen. That’s serious and sometimes requires hospitalization.
In vitro fertilization (IVF) is the last resort for most. PCOS patients respond strongly to IVF drugs, but they need lower doses than other women to avoid OHSS. Even then, the risk of OHSS is still 10 to 20%, compared to 1 to 5% in non-PCOS patients. Still, IVF gives the highest chance of pregnancy per cycle-around 40 to 50%-especially if there are other fertility issues like blocked tubes or male factor infertility.
What No One Tells You About PCOS Treatment
Most treatment plans ignore the emotional toll. On online forums like Reddit’s r/PCOS, women share stories of waiting years for a diagnosis, being told their symptoms were "just stress," or being blamed for their weight. A 2022 survey found that 78% of women with PCOS felt judged for their weight during medical visits. That stigma makes people avoid doctors, delaying care even more.
Another hidden problem? Lack of nutrition guidance. Only 32% of women with PCOS get proper dietary advice, even though low-glycemic diets (foods that don’t spike blood sugar) can reduce insulin levels by 30%. The DASH diet, designed for high blood pressure, has also been shown to improve menstrual regularity by 35% in just 12 weeks. And it’s not just about food-sleep, stress, and movement matter too. One woman on BabyCenter shared that after three failed Clomid cycles, letrozole worked on the first try-and she got pregnant with twins at 32. But she also credits daily walks and cutting out sugary drinks.
And then there’s the long game. PCOS doesn’t go away after pregnancy. Women with PCOS are two to four times more likely to develop type 2 diabetes by age 40. Their risk of heart disease is doubled. That’s why experts now say PCOS isn’t just a fertility issue-it’s a lifelong metabolic condition. Annual blood tests for glucose and cholesterol aren’t optional. They’re essential.

New Hope: What’s on the Horizon
The future of PCOS care is personal. No two women have the same mix of symptoms. Some struggle mostly with weight and insulin. Others have severe acne and hair growth but normal weight. New research is grouping PCOS into subtypes so treatment can match the problem, not just the label.
AI is stepping in too. Algorithms using blood markers like AMH (anti-Müllerian hormone), LH:FSH ratios, and ovarian volume are already 92% accurate at predicting PCOS-faster and cheaper than waiting for ultrasounds. In 2022, the FDA approved Femaloop PCOS, a digital app that gives personalized diet, exercise, and sleep plans. In trials, it improved menstrual regularity by 28% over six months.
And new drugs are coming. Relugolix, combined with estrogen and progesterone, is in phase III trials and has shown 89% menstrual regularity compared to 32% with placebo. It could be the first drug to directly fix the hormonal imbalance instead of just chasing ovulation.
What You Can Do Today
If you suspect PCOS, don’t wait. Track your periods. Note any hair growth, acne flare-ups, or weight changes. Ask for a blood test for testosterone, LH, FSH, insulin, and fasting glucose. Get an ultrasound only if your doctor thinks it’s necessary-especially if you’re under 18, since normal teenage ovaries can look polycystic.
Start with small steps: swap white bread for whole grain, walk 20 minutes a day, cut out sugary drinks. Talk to a dietitian who understands PCOS. If you’re trying to conceive, ask about letrozole before Clomid. And remember: your worth isn’t tied to your ability to get pregnant. PCOS is a medical condition, not a personal failure. With the right support, most women with PCOS go on to have healthy pregnancies-and live healthy lives long after.



Brian Bell
November 14, 2025 AT 18:05Eleanora Keene
November 15, 2025 AT 00:15Ryan Anderson
November 15, 2025 AT 17:52Kevin Wagner
November 16, 2025 AT 07:14gent wood
November 18, 2025 AT 00:50Hrudananda Rath
November 19, 2025 AT 14:03Jane Johnson
November 21, 2025 AT 00:58Sean Hwang
November 22, 2025 AT 09:07Don Ablett
November 23, 2025 AT 00:33Nathan Hsu
November 24, 2025 AT 19:00Peter Aultman
November 26, 2025 AT 17:22Dilip Patel
November 28, 2025 AT 13:41Ashley Durance
November 29, 2025 AT 04:26Scott Saleska
November 29, 2025 AT 19:27Joe Goodrow
November 30, 2025 AT 14:06