
When someone you love is taking five, six, or even ten different medications every day, keeping track isn’t just helpful-it’s life-saving. Over 40% of older adults in the U.S. are managing multiple prescriptions, and for caregivers, that means juggling pills, doses, timing, side effects, and doctor changes-all while trying to keep things calm and safe at home. A simple, well-organized medication list cuts through the chaos. It prevents dangerous mix-ups, stops duplicate prescriptions, and gives doctors the full picture during emergencies. This isn’t about being perfect. It’s about being prepared.
What Goes on a Medication List
A good medication list doesn’t just say "take blood pressure pill." It gives you the details you need when it matters most. Every medication, whether prescription, over-the-counter, or supplement, needs six key pieces of information:- Full name-both brand and generic (e.g., "Lisinopril (Zestril) 10mg")
- Dosage-how much to take each time (e.g., "1 tablet")
- Frequency-how often (e.g., "once daily," "every 8 hours as needed")
- Purpose-why it’s being taken (e.g., "for high blood pressure," "for joint pain")
- Special instructions-"take with food," "don’t crush," "avoid alcohol," "store in fridge"
- Prescriber and pharmacy-doctor’s name and pharmacy phone number
Don’t forget allergies. Listing known reactions-like "penicillin causes rash" or "ibuprofen causes stomach bleeding”-can prevent serious harm. The FDA says this single step stops over 1.3 million adverse reactions each year. Also include the start date for each medication. If something was prescribed for just two weeks but kept going, that’s a red flag. Many seniors end up taking pills long after they’re needed because no one checked.
Why Paper Still Matters (Even in a Digital World)
Digital apps like Medisafe or MyMeds are great-they send reminders, track refills, and sync with pharmacies. But when the power goes out, the phone dies, or someone’s rushed to the ER, a paper list is the only thing that works. Sixty-three percent of caregivers still rely on handwritten or printed lists, and for good reason. In emergencies, first responders don’t ask for your app login. They ask for a list.Here’s how to make a paper list that actually helps:
- Use a clean, large-font template (the FDA’s "My Medicines" form is free to download)
- Laminate it or put it in a clear plastic sleeve
- Keep it in a fixed spot-front pocket of a wallet, taped to the fridge, or in a small binder with other medical papers
- Include a photo of each pill next to its name if memory is an issue. One caregiver on Reddit shared how adding pictures of her mother’s pills cut errors by 65% in six months
Don’t write on the list with pencil. Use a permanent marker. If you need to update it, make a new copy. Scribbles and corrections lead to confusion. And always keep at least two copies-one at home, one with the caregiver or a trusted family member.
When to Use Digital Tools
If the person you’re caring for takes more than four medications, digital tools become a game-changer. Studies show digital lists reduce dosing errors by 42% compared to paper alone. But not all apps are created equal. Many are too complex for older users.Look for apps with:
- Large buttons and simple menus
- Voice input options (say "Add Lisinopril 10mg once a day" instead of typing)
- Automatic refill alerts tied to your pharmacy
- Ability to email or print the list instantly
CVS and Walgreens now offer free medication synchronization-when you refill one prescription, they update your digital list across all others. That’s huge. It cuts update time by 75%. If you’re already using one of these pharmacies, sign up. No extra cost. No app download needed-just ask at the counter.
But here’s the catch: 71% of caregivers stop using apps within three months. Why? Too much work. If you’re spending 20 minutes a week entering data, you’ll quit. The trick? Use the app as a backup, not your main system. Let the pharmacy sync what they know. Then manually add supplements, OTC meds, and special notes. That’s it.
The Brown Bag Method
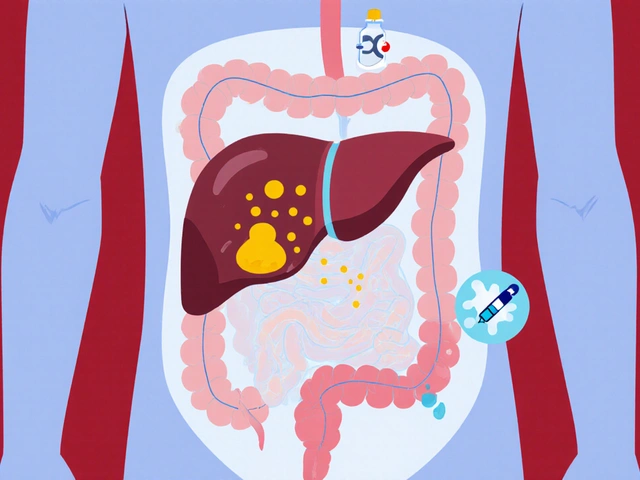
One of the most powerful tools you have? A brown paper bag. Every time you go to a doctor’s appointment-whether it’s the primary care physician, cardiologist, or even the dentist-bring every single medication your loved one is taking. Pills, patches, liquids, vitamins, herbal teas-all of it. Put them in a bag and hand it to the provider.This simple act reveals hidden problems:
- Two doctors prescribed the same drug without knowing
- A supplement interacts dangerously with a prescription
- Old prescriptions were never stopped
AARP found that 89% of caregivers who used the brown bag method said it was "extremely helpful" for appointments. It’s not glamorous. But it works. Do it every time. Even if you think you’ve updated the list. People forget. Doctors miss things. The bag doesn’t lie.
How to Keep It Updated
A medication list is useless if it’s outdated. Studies show 78% of hospital readmissions for seniors happen because their medication list didn’t match what they were actually taking.Set a weekly ritual. Pick a day-Sunday evening works for most people-and spend 15 minutes checking:
- Did any prescriptions change this week?
- Did the pharmacy switch a brand to generic?
- Was a new OTC medicine bought? (Aspirin, melatonin, cough syrup-add them)
- Was a dose skipped or changed?
Update both the paper and digital versions at the same time. If you don’t, they’ll drift apart. And when they do, confusion follows.
For "as needed" medications-like painkillers or anti-anxiety pills-create a separate PRN log. Write down when each one was taken, how much, and why. This helps spot patterns: "She took 4 Tylenol yesterday because she couldn’t sleep. Was it the pain or the anxiety?"
Who Should See the List
Your list isn’t just for you. It’s for everyone involved:- Primary care doctor-review it every 3 months
- Pharmacist-ask them to check for interactions. Most will do it for free
- Specialists-cardiologist, neurologist, etc.-each should have a copy
- Emergency contacts-give one to a neighbor, family member, or friend
- Hospital staff-hand it to the nurse on admission
There’s a growing law called the Caregiver Advisee Act. It requires hospitals to give caregivers a copy of the updated medication list before discharge. But don’t wait. Bring your own. If the hospital gives you a list, compare it to yours. If they’re different, ask why.

Common Mistakes and How to Fix Them
Here’s what goes wrong-and how to avoid it:- Mixing up similar-sounding names-Lisinopril and Lasix? Write them clearly and add the purpose. "Lisinopril-blood pressure. Lasix-water pill."
- Ignoring supplements-Fish oil, vitamin D, turmeric-they’re not "just vitamins." They interact with drugs. Treat them like prescriptions.
- Not knowing why a pill is taken-If you don’t know, call the pharmacist. 68% of caregivers say they don’t understand the purpose of some meds. Don’t guess.
- Forgetting to update after hospital stays-Discharge papers often change meds. Update your list the same day.
- Using abbreviations-"QD" or "BID"? Write "once daily" and "twice daily." No one remembers medical shorthand in a crisis.
What Experts Say
Dr. Sarah Ahmed, a geriatric pharmacist at Johns Hopkins, says a good list reduces duplicate prescriptions by 31% and catches inappropriate meds in 27% of cases. The American Geriatrics Society says every list should include a "stop date" for time-limited prescriptions. If a pill was meant for 14 days and it’s still in the bottle after three months, it’s time to ask: "Do we still need this?"Pharmacists recommend writing the National Drug Code (NDC) number for each medication. It’s the 11-digit barcode number on the bottle. It’s not just for professionals-it helps avoid dispensing errors. You can find it on the label or ask your pharmacist for it.
And here’s the big one: Review the entire list with a pharmacist every three months. Not your doctor. A pharmacist. They’re trained to spot interactions, unnecessary drugs, and dosing risks. Most pharmacies offer this for free. Just ask.
Final Tip: Make It a Team Effort
You don’t have to do this alone. Sit down with family members. Assign roles:- One person handles pharmacy refills
- One updates the list after doctor visits
- One keeps the brown bag ready
- One checks the list every Sunday
When it’s shared, it’s sustainable. And when it’s accurate, it’s safe.
Organizing a medication list isn’t about perfection. It’s about protection. One clear, current, and accessible list can prevent a hospital stay, a bad reaction, or even a death. Start today. Gather the pills. Write the names. Call the pharmacy. And keep going. Every small step matters.
What’s the most important thing to include on a medication list?
The most important thing is the full name (brand and generic), exact dosage, frequency, and purpose of each medication. Without this, doctors and pharmacists can’t tell if a pill is safe or if it’s being taken correctly. Also include allergies-this alone prevents over a million adverse reactions each year.
Should I use a paper list or an app?
Use both. A paper list is essential for emergencies when phones die or power goes out. A digital app helps with reminders and syncing refills. The best approach is a laminated paper list kept in an easy-to-find spot, plus a simple app like Medisafe or the free tool from your pharmacy as a backup.
How often should I update the medication list?
Update it immediately after any change-new prescription, stopped pill, dosage change, or new supplement. Then do a full weekly check every Sunday. Even if nothing changed, review each item. Many errors happen because people forget to remove old meds.
Do I need to include vitamins and supplements?
Yes. Supplements like fish oil, vitamin D, or herbal remedies can interact with prescription drugs. They’re not harmless. Treat them exactly like medications: list the name, dose, frequency, and why you’re taking them. Many hospital errors happen because supplements were left off the list.
What should I do if my loved one is hospitalized?
Bring the full medication list and the brown bag of all pills to the hospital. Give the list to the admitting nurse and ask them to compare it with what’s in the system. When discharged, get the updated list and check it against your own. If anything’s missing or changed, ask why. Hospital staff often miss or misrecord medications during transitions.
Can I trust what the pharmacy tells me about my meds?
Pharmacists are your best allies. They see all your medications together and can spot dangerous interactions you might miss. Ask them to review the list every three months. Most pharmacies offer this for free. Don’t wait for a problem-get the review done proactively.



james thomas
November 11, 2025 AT 09:26Look, I get it - paper lists are ‘reliable,’ but this whole thing is so 2003. If your grandma can’t use a smartphone, that’s a family problem, not a medical one. I’ve seen people die because they brought a hand-written list to the ER and the nurse misread ‘Lisinopril’ as ‘Lisinopril 20mg’ - because someone scribbled it in pencil. Digital is the future. Stop romanticizing paper. It’s just nostalgia with side effects.
Asia Roveda
November 12, 2025 AT 07:20Let’s be real - the government’s been pushing this ‘medication list’ crap since 2010. Meanwhile, Big Pharma is still pushing polypharmacy on seniors like it’s a loyalty program. You think a laminated list stops them from prescribing 12 new pills after a 12-minute visit? Please. The real issue is the system. Not your paper.
Micaela Yarman
November 14, 2025 AT 03:01It is with profound respect for the dignity of elderly care that I submit the following observation: the institutionalization of medication management through standardized documentation is not merely a practical necessity - it is an ethical imperative. The absence of a comprehensive, legible, and universally accessible pharmaceutical inventory constitutes a systemic failure in patient advocacy. I urge all caregivers to adopt the FDA’s My Medicines form as a sacrament of responsibility.
mohit passi
November 15, 2025 AT 14:43bro this is life or death 🙏
my uncle took 2 blood pressure pills by accident because the label was blurry
now he’s fine but i cried for 3 hours
just write it down. use a notebook. take a pic. do something. you don’t need fancy apps. just don’t ignore it. ❤️
Brittany Medley
November 16, 2025 AT 20:42I’ve been a caregiver for 7 years. I’ve seen everything - from people forgetting their own name to overdosing on melatonin because they thought ‘natural’ meant ‘safe.’ This list? It’s not optional. I keep mine in a plastic sleeve taped to the fridge, next to the cat’s vaccination record. And yes - I use permanent marker. And yes - I update it every Sunday. No exceptions. No drama. Just survival.
Rachel Whip
November 17, 2025 AT 18:11One thing no one talks about: the emotional weight of this. It’s not just about writing down pills - it’s about holding someone’s life in your hands. Every time I update the list, I feel it. I’m not just a caregiver. I’m the keeper of their rhythm. So yeah, I’ll laminate it. I’ll take photos. I’ll bring the brown bag. Because if I don’t, who will?
Ezequiel adrian
November 18, 2025 AT 14:24you people are overcomplicating this
just take all the bottles to the doctor
they don't care about your app or your laminated paper
they care about what's in the bag
simple. done. stop reading blogs and just DO IT
Deborah Williams
November 19, 2025 AT 14:22Oh, so now we’re assigning ‘roles’ to family members like it’s a corporate retreat? ‘One person handles pharmacy refills’? Cute. Meanwhile, Aunt Linda is still taking her ex-husband’s leftover Xanax because ‘it helps with the anxiety’ and no one’s dared to ask why. This list won’t fix family dysfunction. It’ll just make you feel better about ignoring it.
Joe bailey
November 21, 2025 AT 03:50Man, I just lost my dad last year. He had 8 meds. I had no idea what half of them did. I wish I’d known about the brown bag thing sooner. I didn’t even know he was taking fish oil until I found the bottle behind the toilet. I wish I’d asked more. I wish I’d written it down. Don’t wait like I did. Start today. Even if it’s just one pill. One line. One step. It matters.
Stephen Adeyanju
November 22, 2025 AT 05:25THEY’RE DRUGGING OUR GRANDMAS
THEY WANT YOU TO THINK THIS LIST IS THE ANSWER
BUT THE REAL PROBLEM IS THE SYSTEM
THEY’RE PROFITING OFF YOUR PARENTS’ PAIN
THEY WANT YOU TO BE TOO BUSY TO NOTICE
THEY WANT YOU TO THINK A LAMINATED SHEET CAN FIX A BROKEN HEALTHCARE MACHINE
STOP COLLABORATING WITH THE MACHINE
BURN THE LIST
AND THE APP
AND THE PHARMACY
AND THE DOCTOR
AND JUST…
LET THEM DIE IN PEACE
Aaron Whong
November 23, 2025 AT 22:30The ontological burden of polypharmacy in geriatric populations is exacerbated by epistemic fragmentation across care domains. The paper-based paradigm, while phenomenologically reassuring, is structurally incommensurate with the distributed cognitive architecture required for longitudinal pharmacovigilance. Digital integration, when mediated through interoperable EHR systems with NDC-based reconciliation protocols, constitutes the only viable path toward epistemic coherence in medication management. The brown bag method, while emotionally resonant, remains a heuristic artifact of pre-digital epistemic regimes.
Sanjay Menon
November 25, 2025 AT 08:04Let’s be honest - this whole thing is performative. You laminate your list, post it on Instagram with #CaregiverLife, and feel like a hero. Meanwhile, your mom’s still taking that expired statin because ‘it’s just one pill.’ The system doesn’t care. The hospital doesn’t care. Your ‘team effort’? It’s just guilt dressed up as organization. You’re not saving lives. You’re curating a narrative.
Marissa Coratti
November 25, 2025 AT 22:00As someone who has meticulously documented every medication, supplement, and over-the-counter intervention for my mother over the past eight years - including the precise time of administration, the ambient temperature of storage, and the emotional context of each dose (e.g., ‘took at 8:17 p.m. after crying because she thought she’d forgotten my birthday’) - I can confidently assert that the true value of this practice lies not in its utility for medical professionals, but in its function as a ritual of love. Each entry is a testament to presence. Each update, a whisper: I am still here. I have not forgotten you. And if, in the chaos of modern healthcare, this is the only thing that remains - then perhaps, in the end, it is enough.