
Long COVID Treatment Risk Calculator
How This Tool Works
This calculator helps you understand potential benefits and risks of different Long COVID treatments based on your specific symptoms, health conditions, and current medications. Note: This is NOT medical advice. Always consult your doctor before starting any treatment.
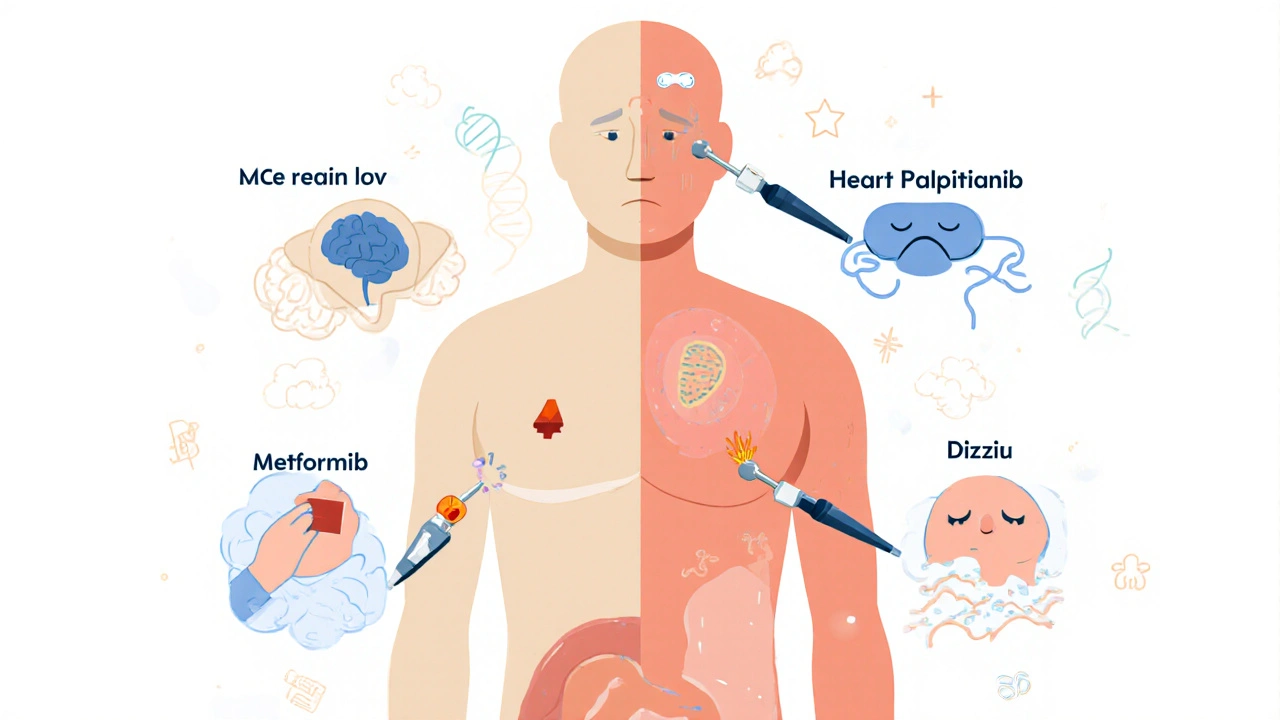
More than 15 million people in the U.S. alone are living with Long COVID - symptoms that won’t go away weeks or months after the initial infection. Fatigue, brain fog, heart palpitations, dizziness, and shortness of breath are just a few of the 200+ documented symptoms. There’s no FDA-approved treatment yet. So people are turning to medications not designed for this condition, hoping something might help. But what are they taking? And more importantly, are these drugs safe for them?
Baricitinib: A Rheumatoid Arthritis Drug With Serious Risks
Baricitinib is one of the most studied drugs for Long COVID right now. It’s a JAK inhibitor approved for rheumatoid arthritis and alopecia areata. It was even used during the height of the pandemic to reduce deaths in hospitalized COVID patients. Now, it’s being tested in the REVERSE-LC trial - a major NIH-funded study with over 40 researchers across six sites.
The theory? Long COVID may involve chronic inflammation, and baricitinib dampens immune overactivity. Early signals from smaller trials looked promising. But here’s the catch: baricitinib carries real dangers. In rheumatoid arthritis patients, serious infections happened in 10-20% of users. The risk of lymphoma and major heart events is also elevated - 3.3 to 4.1 events per 100 patient-years, according to the FDA label. These aren’t rare side effects. They’re documented, predictable, and potentially life-threatening.
Most Long COVID patients aren’t elderly or immunocompromised like those in rheumatoid arthritis trials. They’re often younger, previously healthy people. That means the safety profile we know might not apply. Could their immune systems react differently? We don’t know yet. The trial results are expected in late 2026. Until then, prescribing baricitinib outside of a clinical trial is off-label and risky.
Metformin: The Most Promising Option - With a Gut Problem
If you’re looking for the strongest evidence so far, metformin stands out. A 2023 University of Minnesota trial published in Nature Medicine found that people who took metformin within four days of a positive COVID test had a 41% lower chance of developing Long COVID. That’s not a small effect. It’s statistically significant and clinically meaningful.
Metformin is cheap, widely available, and has been used safely for decades to treat type 2 diabetes. But its side effects are hard to ignore. In that same trial, 35.7% of participants had gastrointestinal issues - nausea, diarrhea, bloating. That’s more than one in three. For someone already battling fatigue and brain fog, these symptoms can make life worse, not better.
Some doctors are prescribing it anyway. A 2025 survey from the Body Politic Long COVID Support Group showed 32% of respondents had tried metformin. But 57% said it didn’t help enough, and 41% said the side effects were worse than their Long COVID symptoms. It’s a trade-off. For some, the benefit outweighs the discomfort. For others, it’s unbearable.
Low-Dose Naltrexone: A Quiet Hope With Hidden Costs
Low-dose naltrexone (LDN) isn’t new. It’s been used off-label for decades for autoimmune conditions, chronic pain, and fatigue. Doses are tiny - 1 to 5 mg daily - compared to the 50 mg used for opioid addiction. At this level, it’s thought to modulate inflammation and reset immune signaling.
A 2024 observational study from Nova Southeastern University tracked 120 Long COVID patients on LDN. Sixty-two percent reported improved energy. That’s encouraging. But side effects popped up too: 28% had trouble sleeping. 19% got headaches. These aren’t minor. Sleep disruption alone can worsen brain fog and fatigue - the very symptoms people are trying to fix.
There’s no large-scale trial yet. No randomized control group. Just patient reports. That means we can’t say LDN works. We can only say some people feel better. And some feel worse. Without clear dosing guidelines or long-term safety data, using LDN feels like stepping into the dark with a flashlight.
Paxlovid: The Antiviral That Might Not Work - And Its Bitter Taste
Paxlovid - nirmatrelvir/ritonavir - is the go-to antiviral for early COVID. But does it help with Long COVID? Two big studies say no.
A small UCSF study in 2024 showed symptom improvement in 38% of patients on a 15-day course, compared to 22% on placebo. That sounded hopeful. Then came the NIH’s larger RECOVER trial in early 2025. It found no difference between Paxlovid and placebo: 34.1% vs. 32.8%. Statistically, it’s noise.
And then there’s the taste. Seventy-nine percent of users reported a lingering, metallic, bitter aftertaste. Some said it made them nauseous. Others couldn’t eat for hours after taking it. And ritonavir - the booster in Paxlovid - interacts with over 100 common medications. Blood thinners, statins, anxiety meds, even some heart drugs. For someone already on multiple prescriptions, Paxlovid could be dangerous.
It’s not the answer. Not yet. And it’s not safe for everyone.
What’s on the Horizon - And What Failed
Not every experiment has gone well. BC007, a drug meant to neutralize harmful autoantibodies linked to Long COVID, was halted in March 2025 after a phase II trial showed no benefit over placebo. Three serious infusion reactions occurred in the treatment group - one more than placebo. That’s a red flag.
Other drugs are still in early testing. AstraZeneca’s sipavibart, a monoclonal antibody approved for COVID prevention in Europe and Japan, is now being tested for Long COVID. But safety data? Only from prevention use - injection site reactions in 15%, rare allergic responses. No data yet on how it affects fatigue or brain fog.
Then there’s tirzepatide (Mounjaro), a diabetes and weight-loss drug. Early theories suggest it might help with metabolic dysfunction and brain inflammation in Long COVID. But its side effects - nausea, vomiting, diarrhea - are similar to metformin’s. Will it help, or just add to the suffering?
And what about stellate ganglion blocks? A nerve procedure used for chronic pain. Some clinics are offering it for Long COVID-related dizziness and heart rate issues. Early reports say 15% get hoarseness. 5% get a hematoma. No large studies. No long-term data. Just anecdotal hope.

The Big Unknowns
We don’t know what causes Long COVID. Is it lingering virus? Autoimmunity? Damaged blood vessels? Broken mitochondria? All of the above? Without knowing the root cause, we’re guessing at treatments.
We don’t have biomarkers. No blood test, no scan, no clear signal to tell who will respond to what. That’s why trials fail. You can’t give a drug to someone who might not even have the condition you’re trying to treat.
We don’t know who should take what. A 25-year-old athlete with brain fog needs a different approach than a 60-year-old with heart rhythm issues. The NIH now recognizes at least four distinct Long COVID subtypes. One drug won’t fit all.
And we don’t know the long-term safety. Baricitinib’s risks were seen in arthritis patients over years. What happens if a healthy 30-year-old takes it for six months? Two years? We’re flying blind.
What Should You Do?
If you’re considering a medication for Long COVID, talk to your doctor - but don’t expect clear answers. There are no guidelines. No consensus. The American Medical Association admits that in January 2025.
Ask about clinical trials. The NIH’s RECOVER initiative is running dozens. These aren’t just research projects - they’re safer than self-experimenting. You get monitored. You get data. You’re not alone.
If you’re taking something off-label, track your symptoms. Keep a log: what you took, when, how you felt, side effects. Share it with your provider. Your experience matters - especially when science hasn’t caught up.
And be cautious. The promise of relief can make people ignore red flags. A 2025 survey found 41% of people who tried medications said the side effects were worse than their Long COVID. That’s not progress. That’s a trade-off with no payoff.
The first FDA-approved Long COVID treatment might come by 2027 or 2028. But until then, the field is a minefield. Every drug has a signal. Every signal has a cost. The goal isn’t just to find something that works. It’s to find something that works - without breaking something else.
Is there any FDA-approved treatment for Long COVID yet?
No, there are currently no FDA-approved medications specifically for Long COVID. All current treatments are off-label or experimental, meaning they’re being used for a purpose other than what they were originally approved for. Clinical trials are ongoing, and the first approvals may not come until late 2027 or 2028.
Can I safely take metformin for Long COVID on my own?
While metformin shows promise in reducing Long COVID risk when taken early after infection, it’s not without risks. Gastrointestinal side effects like nausea and diarrhea affect over one-third of users. Taking it without medical supervision could worsen symptoms or interact with other medications. Always consult a doctor before starting metformin, even if it’s available over the counter in some countries.
Why do some doctors recommend baricitinib while others warn against it?
Some doctors see baricitinib’s success in treating acute COVID as a reason to try it for Long COVID, especially since inflammation may play a role. Others warn that Long COVID patients aren’t the same as those with rheumatoid arthritis - they’re often younger and not immunocompromised. The safety data we have doesn’t fully apply, and the risk of serious infections or heart events could outweigh benefits. The debate reflects the lack of clear evidence, not a settled consensus.
Are there any safe, non-medication options for Long COVID?
Yes. Pacing - managing activity levels to avoid post-exertional malaise - is the most widely recommended non-medication strategy. Graded exercise is not advised for most, as it can worsen symptoms. Cognitive behavioral therapy (CBT) tailored for Long COVID, sleep hygiene, and hydration are also supported by patient and clinical experience. These don’t cure, but they can help manage daily function and reduce symptom spikes.
How can I find a clinical trial for Long COVID treatments?
The NIH’s RECOVER initiative lists active trials on its website, and many are recruiting. You can also search ClinicalTrials.gov using terms like “Long COVID,” “PASC,” or specific drug names like “baricitinib” or “metformin.” Many trials cover travel costs and provide free medical monitoring. Participating helps science - and gives you access to treatments not yet available to the public.




Jackson Olsen
October 30, 2025 AT 13:06Metformin gave me serious stomach issues but honestly? My brain fog cleared a bit. Still taking it, just slower now. 🤷♂️
Penny Clark
November 1, 2025 AT 11:17i tried ldn and slept worse but my heart palpitations slowed down?? idk man. it’s a gamble. 🫠
Niki Tiki
November 3, 2025 AT 02:44why are we giving diabetic drugs to healthy people this is america not a lab experiment
Jim Allen
November 4, 2025 AT 21:28baricitinib sounds like a bad idea unless you wanna get a serious infection and then explain to your family why you took a rheumatoid arthritis pill because a reddit post said so
Nate Girard
November 4, 2025 AT 22:01if you’re thinking about trying anything off-label please track your symptoms. i started a google sheet and it helped me see what actually helped vs what felt like hope. we need more data from real people not just trials.
Carolyn Kiger
November 5, 2025 AT 09:40pacing saved me. not drugs. just learning to say no to plans and rest when my body screams. it’s boring but it’s real.
krishna raut
November 6, 2025 AT 06:45metformin works for some. side effects are real. but long covid is worse. consult doctor.
Prakash pawar
November 7, 2025 AT 17:53you people are so scared of science why not just take the pill and see what happens life is risk anyway
MOLLY SURNO
November 9, 2025 AT 03:29Thank you for sharing this comprehensive overview. The lack of clear guidelines is deeply frustrating for patients. I appreciate the emphasis on clinical trials - they offer both safety and contribution to future solutions.
Alex Hundert
November 9, 2025 AT 16:22LDN didn’t help me but the sleep issues? That’s the real cost. I’d rather be tired than foggy. Now I’m trying pacing + hydration. No magic bullet, just small wins.
Emily Kidd
November 10, 2025 AT 09:47took metformin for 3 weeks. diarrhea every day. stopped. still have brain fog. but at least i can poop now. 😅