
Heart disease isn’t just something that happens to older people. It’s the leading cause of death worldwide, killing nearly 18 million people each year. And here’s the hard truth: heart disease risk factors aren’t random. They’re predictable. Some you can’t change. Others? You can fix them-today.
What You Can’t Change: Age, Sex, and Family History
You can’t turn back time. And you can’t change your genes. But knowing how these factors affect your heart lets you prepare. Men over 45 and women over 55 see their risk climb sharply. By age 70, about 7 in 10 men and 6 in 10 women will develop heart disease. That’s not fate-it’s biology.Family history is even more telling. If your parent or sibling had a heart attack before age 55 (for men) or 65 (for women), your risk jumps by 60% to 75%. It’s not just bad luck. Specific genes, like the 9p21 variant, can increase your risk by 20-30% per copy. And then there’s familial hypercholesterolemia-a silent genetic disorder affecting 1 in 250 people. Left untreated, it can lead to a heart attack before 50.
Women face a unique twist. Before menopause, estrogen offers some protection. After, that shield fades. By age 65, a woman’s risk matches a man’s. And racial disparities are real: African Americans die from heart disease at 30% higher rates than non-Hispanic whites. It’s not about willpower-it’s about biology and access.
What You Can Change: The Big Four
The good news? Up to 80% of early heart disease is preventable. You don’t need a miracle. You need to tackle the big four: smoking, high blood pressure, high cholesterol, and inactivity.Smoking is the single most preventable cause. Even five cigarettes a day raises your heart disease risk by 50%. Smoking damages your arteries, thickens your blood, and spikes your blood pressure. Quitting cuts your risk in half within a year. After 15 years, it’s nearly the same as someone who never smoked.
High blood pressure affects nearly half of American adults. If your systolic number is above 130, your heart is working too hard. Uncontrolled, it triples or quadruples your risk. The SPRINT trial showed that lowering it to under 120-instead of the old 140-cuts heart attacks and strokes by 25%. That’s not a suggestion. It’s a medical imperative.
High cholesterol is another silent killer. LDL-the bad kind-builds up in your arteries. If your LDL is above 100, you’re in danger. People with levels above 160 have 50% higher risk than those with optimal levels. Statins aren’t magic pills, but they reduce heart attacks by 25-35% in high-risk patients. They’re not for everyone, but for many, they’re life-saving.
Physical inactivity is just as dangerous as smoking. People who sit all day have a 30% higher risk of heart disease than those who move regularly. You don’t need to run marathons. Just 150 minutes a week of brisk walking-about 30 minutes, five days a week-cuts your risk significantly.
The Hidden Players: Diabetes, Weight, and Stress
Diabetes doesn’t just affect your blood sugar. It wrecks your blood vessels. People with diabetes are two to four times more likely to die from heart disease. And here’s the kicker: 68% of diabetics over 65 die from heart problems. Managing blood sugar isn’t just about insulin-it’s about protecting your heart.Obesity isn’t just about appearance. Belly fat releases chemicals that inflame your arteries. Losing just 5-10% of your body weight can lower blood pressure, improve cholesterol, and reduce insulin resistance. It’s not about perfection. It’s about progress.
Stress and sleep? They matter. Chronic stress raises cortisol, which bumps up blood pressure and inflammation. Poor sleep-less than six hours a night-doubles your risk of high blood pressure. And loneliness? Studies show it’s as harmful as smoking. Your heart doesn’t just need exercise. It needs connection.
How Risk Multiplies: When One Problem Makes Another Worse
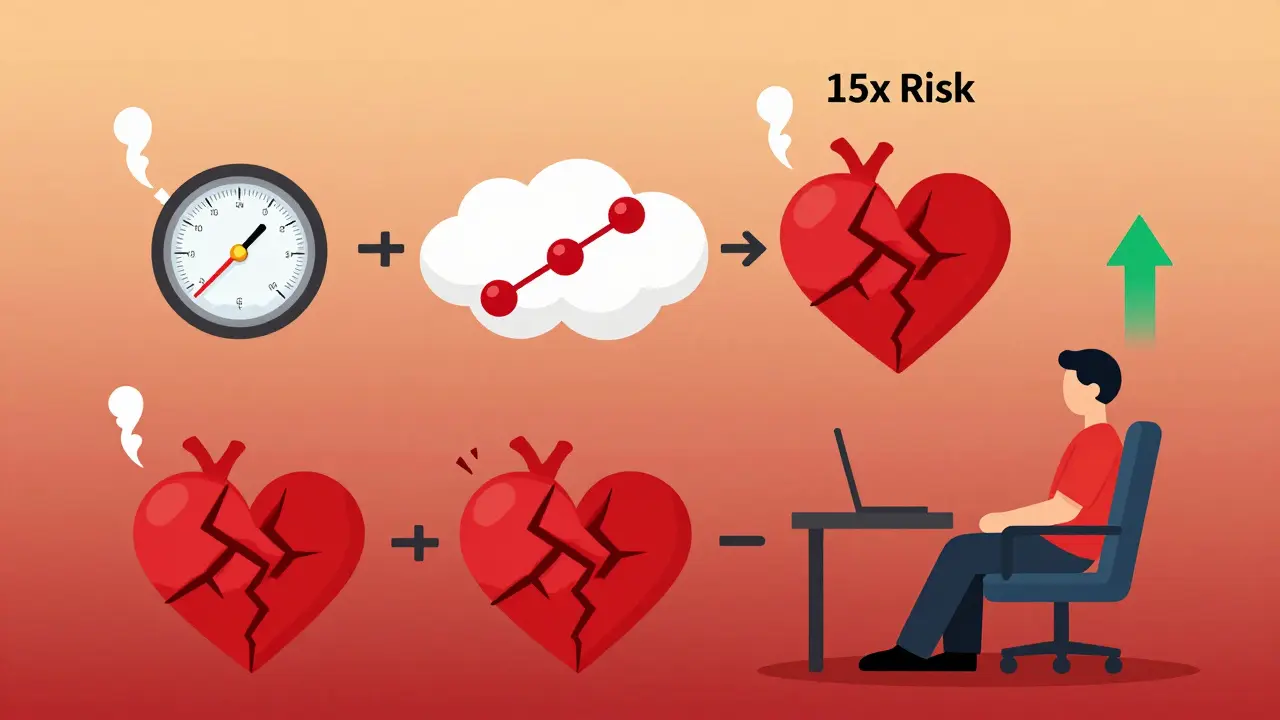
Here’s what most people don’t get: risk factors don’t add up. They multiply.Having both high blood pressure and diabetes? Your heart disease risk jumps 8 to 10 times. Add smoking? It’s worse. Combine all three with obesity? You’re looking at a 15-fold increase. That’s not coincidence. It’s biology working in overdrive.
That’s why the American Heart Association says addressing just three things-smoking, high blood pressure, and inactivity-could prevent nearly half of all heart disease deaths in the U.S. You don’t need to fix everything at once. Start with one. Then another.
Knowing Your Numbers: Tools That Actually Work
You can’t manage what you don’t measure. The American College of Cardiology and American Heart Association use the Pooled Cohort Equations to calculate your 10-year risk. It takes five minutes. You plug in your age, sex, race, cholesterol, blood pressure, diabetes status, and smoking habits. It tells you if you’re low, borderline, intermediate, or high risk.Some doctors now use the Reynolds Risk Score, which adds family history and a simple blood test for inflammation (hs-CRP). That one tweak improves accuracy by 15-20%. If your mom had a heart attack at 52, that’s not just a story. It’s data.
And here’s something new: polygenic risk scores. These genetic tests look at hundreds of tiny DNA variations to predict your inherited risk. If you’re in the top 20%, your risk is 2.5 to 3 times higher-even if your cholesterol is normal. It’s not mainstream yet, but it’s coming fast.
What Works: Real Changes, Real Results
A 48-year-old man in Ohio had it all: smoking, high blood pressure, obesity, and a father who died of a heart attack at 54. His 10-year risk? 18.2%. High. Dangerous.He quit smoking. He started walking 30 minutes a day. He switched to a Mediterranean diet-more veggies, olive oil, fish, less sugar. He took his blood pressure meds. After 18 months, his risk dropped to 6.3%. Not a miracle. Just consistency.
That’s the pattern. People who stick to the ABCS-Aspirin (if prescribed), Blood pressure control, Cholesterol management, Smoking cessation-see dramatic results. The CDC’s Million Hearts initiative has helped millions do exactly that.
What Doesn’t Work: Myths That Cost Lives
You’ve heard them:- “I’m young, so I’m fine.” Wrong. Plaque builds silently for decades.
- “I eat healthy, so I don’t need to check my cholesterol.” False. Genetics can override diet.
- “My dad lived to 90, so I’m safe.” He might have been the exception, not the rule.
- “I’ll quit smoking after the holidays.” Every day you smoke, your arteries are getting worse.
And the worst myth? “I don’t have symptoms, so I’m okay.” Heart disease doesn’t knock. It sneaks in. By the time you feel chest pain, it’s often too late.
Where to Start: Your First Three Steps
You don’t need a plan. You need a start.- Get your numbers: Ask your doctor for a lipid panel, blood pressure check, and fasting glucose test. Don’t wait for a “wellness visit.”
- Write down your family history: Who had heart disease? At what age? Bring that list to your next appointment.
- Choose one habit to change: Walk daily. Cut out sugary drinks. Smoke less. Sleep 7 hours. Pick one. Stick to it for 30 days.
That’s it. No drastic diets. No expensive supplements. Just awareness. And action.
Heart disease isn’t inevitable. It’s avoidable-if you know the risks and act on them. Your heart doesn’t need a hero. It needs you.
Can you have heart disease even if you’re young and fit?
Yes. Genetics, smoking, or undiagnosed high cholesterol can cause heart disease in people under 40. Even athletes can have familial hypercholesterolemia or hidden inflammation. Fitness doesn’t cancel out risk-it just masks it. That’s why knowing your numbers matters more than how you look.
Is family history more important than lifestyle?
No. Family history tells you your starting point, but lifestyle determines your outcome. Someone with a strong family history who eats well, doesn’t smoke, and stays active can have a lower risk than someone with no family history who smokes and is sedentary. Genetics loads the gun. Lifestyle pulls the trigger.
Does quitting smoking really help if I’ve smoked for 30 years?
Absolutely. Within one year of quitting, your heart disease risk drops by half. After five years, your stroke risk matches a non-smoker’s. After 15 years, your risk is nearly the same as someone who never smoked. It’s never too late. Even if you’ve smoked for decades, quitting now gives you more years than continuing.
Should I take aspirin to prevent heart disease?
Only if your doctor says so. Aspirin reduces clotting, which helps some people-but it also increases bleeding risk. For people with no history of heart disease, the risks often outweigh the benefits. Don’t start aspirin on your own. Talk to your doctor about your personal risk profile first.
Can stress or lack of sleep cause heart disease?
Yes, indirectly. Chronic stress raises blood pressure and inflammation. Poor sleep disrupts hormones that control hunger and insulin, leading to weight gain and diabetes-both major heart risks. People who sleep less than six hours a night double their risk of high blood pressure. Managing stress and sleep isn’t optional. It’s part of heart health.
Are cholesterol-lowering drugs safe for long-term use?
Yes, for most people. Statins have been studied for over 30 years. Side effects like muscle pain are rare and often reversible. The bigger risk is not taking them if you need them. For people with high cholesterol or existing heart disease, statins reduce heart attacks and strokes by 25-35%. The benefits far outweigh the risks for those at moderate to high risk.
How often should I get checked for heart disease risk?
Every 4-6 years if you’re healthy and under 40. After 40, or if you have risk factors like high blood pressure, diabetes, or family history, get checked annually. Don’t wait for symptoms. By then, it’s often too late.
Can diet alone lower heart disease risk without medication?
For some, yes. The Mediterranean diet-rich in vegetables, nuts, olive oil, fish, and whole grains-lowers LDL cholesterol, reduces inflammation, and improves blood pressure. Studies show it can cut heart disease risk by up to 30%. But if your risk is high due to genetics or diabetes, diet alone may not be enough. Medication and lifestyle work best together.
Heart disease doesn’t care how busy you are. It doesn’t care if you’re “too young” or “too fit.” It only cares if you know your risks-and if you do something about them. Start today. Not tomorrow. Not next year. Today.




Alex Fortwengler
January 11, 2026 AT 13:49They don’t want you to know this but Big Pharma and the American Heart Association are in bed together. Statins? Totally unnecessary. All you need is turmeric, apple cider vinegar, and praying to the sun. They’re hiding the real cause-EMF radiation from 5G towers frying your arteries. I’ve been tracking this since 2018. My cousin’s dog got heart disease after a Wi-Fi router was installed next to its bed. Coincidence? I think not. 🤡
jordan shiyangeni
January 13, 2026 AT 06:45It is, without a shadow of a doubt, profoundly irresponsible to suggest that lifestyle changes alone can mitigate genetic predispositions without the rigorous, clinically validated, evidence-based intervention that modern cardiology has painstakingly developed over the last half-century. To imply that walking 150 minutes a week is equivalent to addressing familial hypercholesterolemia is not merely misleading-it is a dangerous oversimplification that betrays the very principles of medical science. The data is unequivocal: biological reality does not bend to wishful thinking, and to promote otherwise is to actively endanger public health.
Abner San Diego
January 14, 2026 AT 11:39U.S. healthcare is a scam. You pay $300 for a cholesterol test, then they hit you with a $200/month statin bill. Meanwhile, in China, they eat garlic and walk everywhere and live to 100. We’re not sick because of our genes-we’re sick because we’re lazy and overpriced. Quit smoking? Nah, just buy a $500 ‘heart health’ supplement from a guy on YouTube. That’s the American way. 🇺🇸
Monica Puglia
January 14, 2026 AT 15:15Thank you for writing this. 💙 I’m 32 and my dad had a heart attack at 48. I just got my first lipid panel and my LDL was 142. I’m scared but also… motivated. I started walking after work and swapped soda for sparkling water. Small stuff. But it feels like I’m finally listening to my body. You’re not alone. We got this. 🌱
steve ker
January 14, 2026 AT 15:18Genes rule everything. Your diet means nothing if your DNA says you’re doomed. Stop pretending you can out-eat your parents. The system is rigged. They don’t test for the real markers. You’re being lied to
George Bridges
January 14, 2026 AT 16:17This is one of the clearest, most compassionate summaries of heart disease risk I’ve ever read. I’ve worked with patients who felt hopeless because of family history, and this kind of message-factual but not fatalistic-makes all the difference. Thank you for grounding science in humanity.
Faith Wright
January 15, 2026 AT 08:57Oh wow, so if I’m a 50-year-old woman with a family history and I eat kale and cry into my pillow at night… I’m basically a saint? 🙄 Let me guess-the real villain is my ex who ghosted me and now my cortisol is doing the cha-cha. Maybe if I just meditated harder, my arteries would magically un-clog. I’ll stick with the statin, thanks.
TiM Vince
January 16, 2026 AT 17:47My grandma smoked until 82 and never had a problem. My uncle quit at 45 and had a heart attack two years later. I don’t trust these stats. Everyone’s different. I’ll just keep eating my bacon.
Katherine Carlock
January 17, 2026 AT 23:10Okay but what if you’re broke? I work two jobs, can’t afford a gym, and my only ‘healthy’ food is the free rice at the food bank. You keep saying ‘just walk 30 minutes’-have you ever tried walking after a 12-hour shift with a toddler? This advice is for people who have time and money. Not everyone gets a ‘Mediterranean diet’ upgrade. Just saying.
Sona Chandra
January 19, 2026 AT 19:56THIS IS WHY INDIANS ARE SO HEALTHY WE EAT SPICES AND NEVER GET HEART DISEASE YOU ALL JUST EAT BURGERS AND WATCH NETFLIX
Lelia Battle
January 21, 2026 AT 18:11It is curious how we assign moral weight to health behaviors-quitting smoking as ‘virtue,’ obesity as ‘laziness’-while ignoring the structural forces that shape access to care, nutrition, and time. The individualistic framing of heart disease, however scientifically accurate, risks obscuring the societal failures that make prevention inaccessible to many. Perhaps the real question is not ‘what can you do?’ but ‘what have we allowed to persist?’
Rinky Tandon
January 21, 2026 AT 21:53Polygenic risk scores are the future but nobody is talking about the epigenetic cascade triggered by chronic inflammation from ultra-processed foods and endocrine disruptors in packaging. The AHA is still stuck in the lipid paradigm. You need to measure oxLDL, Lp(a), and hsCRP in tandem with genetic panels. Otherwise you’re flying blind. This is basic cardiovascular pathophysiology 101.
Cassie Widders
January 23, 2026 AT 20:30My dad died at 56. I’m 41 now. I got my numbers checked. LDL was high. So I started walking. No drama. No supplements. Just… walking. It’s not sexy. But it’s something. And I’m still here.
Konika Choudhury
January 24, 2026 AT 19:05Why do they always blame smoking when the real problem is the sugar in your coffee and the stress from your job and the fact that nobody sleeps anymore
Darryl Perry
January 26, 2026 AT 15:13Stop romanticizing lifestyle changes. If you’re at high genetic risk, you need medication. Period. Waiting to ‘try diet first’ is negligent. Your heart doesn’t care how ‘natural’ your diet is. It cares about LDL levels. Get tested. Take the pill. Don’t be a martyr.