Choosing a blood thinner isn’t just about preventing clots - it’s about balancing risk, lifestyle, and long-term safety. For millions of people with atrial fibrillation, deep vein thrombosis, or mechanical heart valves, the decision between warfarin and direct oral anticoagulants (DOACs) can mean the difference between manageable care and life-threatening complications. In 2025, DOACs like apixaban, rivaroxaban, and dabigatran dominate prescriptions, but warfarin still holds critical ground. Understanding the real safety differences isn’t about which drug is ‘better’ - it’s about which one fits your body, habits, and health risks.
How Warfarin Works - And Why It’s Still Around
Warfarin has been the go-to blood thinner since the 1950s. It works by blocking vitamin K, which your body needs to make clotting proteins. Simple in theory, messy in practice. Unlike newer drugs, warfarin doesn’t have a consistent effect from person to person. One dose might be perfect for you, but too strong for your neighbor. That’s why you need regular blood tests - INR checks - to make sure your level stays between 2.0 and 3.0. Too low, and you risk a stroke. Too high, and you could bleed internally without warning.
Over 300 medications interact with warfarin. Even something as simple as eating a big salad or taking an antibiotic can throw your INR off. That’s why people on warfarin often keep food diaries and carry emergency cards. A 2023 study found that only 65% of warfarin users maintain their INR in the safe range more than 70% of the time. For many, that’s not just inconvenient - it’s dangerous.
What Are DOACs - And Why Doctors Now Prefer Them
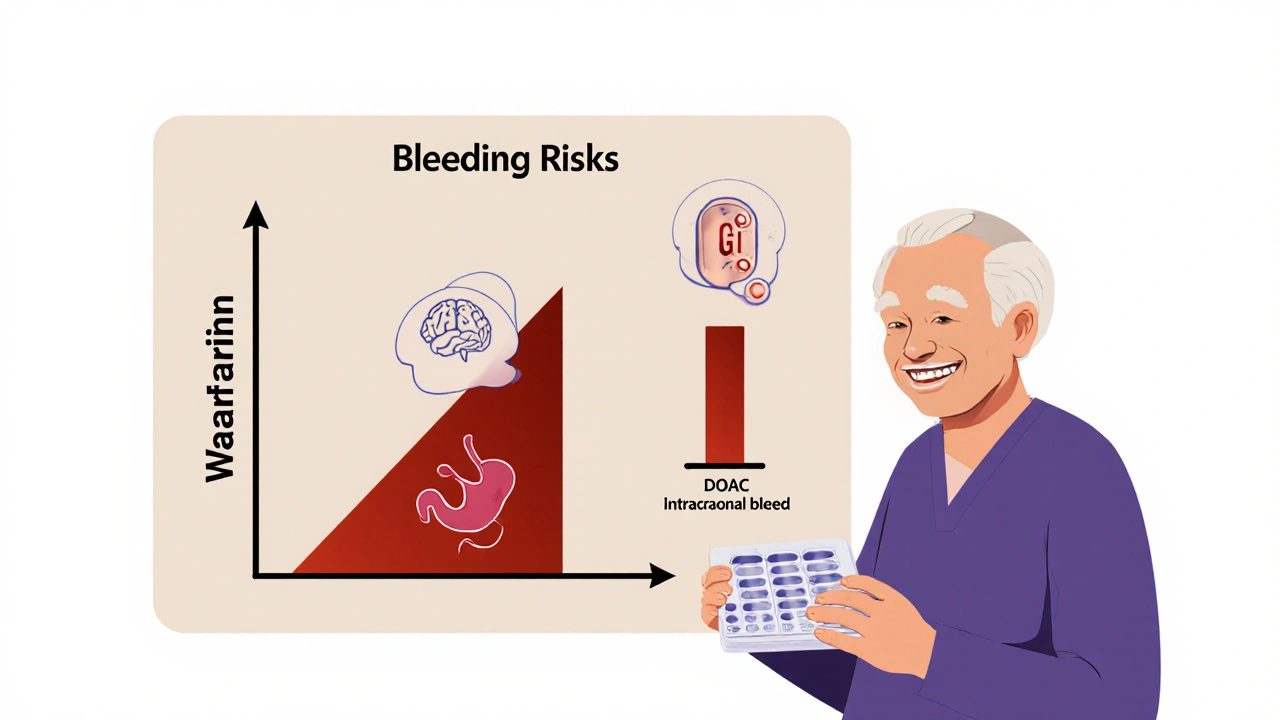
DOACs - apixaban (Eliquis), rivaroxaban (Xarelto), dabigatran (Pradaxa), and edoxaban (Savaysa) - changed the game. They don’t need INR checks. They don’t react with most foods. Their dosing is fixed: once or twice a day, no guessing. In clinical trials, DOACs reduced stroke risk by 20% and intracranial bleeding by 50% compared to warfarin in patients with atrial fibrillation. The American Heart Association now recommends DOACs as first-line for most non-valvular AF cases.
But it’s not magic. DOACs still carry bleeding risks. The difference? The type of bleeding. Warfarin is more likely to cause brain bleeds - the most deadly kind. DOACs tend to cause more gastrointestinal bleeding, which is serious but often less fatal. A 2023 JAMA Network Open study showed DOACs lowered the risk of major bleeding by 18% over five years compared to warfarin. For people over 65, that’s a big win.
Real-World Safety: Who Benefits Most?
Not everyone does better on DOACs. The data shows clear patterns:
- People with kidney problems: DOACs are cleared by the kidneys differently. Dabigatran is mostly removed by kidneys (80%), so it’s risky if your eGFR drops below 30. Apixaban is safer here - only 27% is cleared by kidneys. For patients with severe kidney failure (eGFR <15), warfarin is still the only recommended option.
- People with mechanical heart valves: DOACs are not approved here. A 2023 study showed patients with mechanical valves on DOACs had triple the risk of clotting compared to those on warfarin. This isn’t a preference - it’s a hard rule.
- Younger, active patients: A 2022 Circulation study found younger adults (under 55) had 41% better adherence to DOACs than warfarin. No weekly blood draws. No dietary restrictions. That matters when you’re juggling work, kids, or travel.
- People with cancer: Apixaban showed the lowest bleeding risk in cancer patients with atrial fibrillation. Rivaroxaban didn’t show the same advantage. This isn’t just theory - it’s guiding oncology guidelines now.
Cost, Adherence, and the Hidden Price of Convenience
DOACs cost a lot. Apixaban runs about $587 for a 30-day supply. Warfarin? $4.27. That’s a 140x difference. But cost isn’t just the pill price - it’s the hidden expenses of warfarin: lab visits, time off work, emergency trips for INR spikes. A 2023 analysis found DOACs become cheaper than warfarin when patients miss more than 35% of their INR tests. That’s common. In Medicare data, nearly half of warfarin users don’t get tested regularly.
Adherence is the silent winner. A 2023 study in the American Journal of Managed Care showed DOAC users were 32% more likely to take their medication consistently. For patients aged 18 to 45, that gap jumped to 41%. Missing a dose of warfarin can cause a dangerous INR drop within days. Missing a DOAC dose? Risk rises, but slower - and often without warning signs.
Reversing Bleeding: What Happens When Things Go Wrong
Bad bleeding is rare, but it happens. With warfarin, doctors give vitamin K and fresh frozen plasma. It takes hours to work. With DOACs, there are specific antidotes. Idarucizumab (Praxbind) reverses dabigatran in minutes. Andexanet alfa (Andexxa) reverses apixaban and rivaroxaban. These aren’t just backups - they’re game-changers in emergency rooms. In one 2023 case series, patients on DOACs with major bleeding had a 40% faster time to hemostasis compared to those on warfarin.
But here’s the catch: these reversal agents cost over $20,000 per dose. Hospitals don’t always stock them. If you’re on a DOAC and live far from a trauma center, that’s a real risk. Warfarin’s reversal tools are cheaper and more widely available.

What Your Doctor Won’t Always Tell You
Doctors push DOACs because they’re safer on average. But safety isn’t one-size-fits-all. If you’re on multiple medications - especially antibiotics, antifungals, or seizure drugs - your DOAC levels can spike dangerously. Rivaroxaban interacts with ketoconazole. Apixaban reacts with rifampin. These aren’t rare. One study found 1 in 7 patients on DOACs were taking a drug that could raise bleeding risk.
And what about long-term kidney damage? DOACs are cleared by kidneys, but they don’t cause kidney disease. However, if your kidneys decline over time - say, from diabetes or high blood pressure - you might need to switch. There’s no easy way to predict that. Warfarin doesn’t care about kidney function. It’s a trade-off: convenience now, possible switch later.
Patients with obesity are another gray zone. DOACs are dosed by weight, but most studies didn’t include people over 120 kg. For very heavy patients, some doctors still choose warfarin - not because it’s better, but because they don’t know if DOACs are effective enough.
What Should You Do?
Ask your doctor these five questions:
- Do I have a mechanical heart valve or severe mitral stenosis? If yes, warfarin is your only option.
- What’s my kidney function? (Ask for your eGFR number - not just ‘normal’.)
- Am I on any other meds that could interact? Bring your full list - including supplements.
- Can I afford the DOAC? If not, can we try a generic or patient assistance program?
- How often will I need blood tests? If I can’t commit to monthly INRs, DOACs are safer for me.
If you’re on warfarin and doing well - stable INR, no bleeding, no dietary chaos - don’t switch just because it’s trendy. But if you’re struggling with labs, diet, or missed doses, DOACs are likely a better fit. The data doesn’t lie: for most people, they’re safer, simpler, and more effective.
There’s no perfect anticoagulant. Only the right one for you.
Can I switch from warfarin to a DOAC on my own?
No. Switching anticoagulants requires careful overlap and timing to prevent clots or bleeding. Your doctor will use specific protocols - like running INR tests while starting the DOAC - to ensure safety. Never stop or switch without medical supervision.
Are DOACs safe during pregnancy?
No. DOACs and warfarin both cross the placenta and can harm a developing fetus. If you’re pregnant or planning pregnancy, your doctor will switch you to low-molecular-weight heparin injections, which are safer during pregnancy. This is a critical decision - don’t delay talking to your OB-GYN and cardiologist.
What if I forget a dose of my DOAC?
If you miss a once-daily DOAC and remember within 12 hours, take it right away. If it’s been more than 12 hours, skip the missed dose and take your next one at the regular time. For twice-daily DOACs like apixaban, if you miss a dose within 6 hours, take it. After that, skip it. Never double up. Always check your drug’s specific instructions - they vary.
Do I need to avoid certain foods on DOACs?
Unlike warfarin, DOACs don’t interact with vitamin K-rich foods like leafy greens, broccoli, or Brussels sprouts. You can eat them normally. But avoid large amounts of grapefruit or Seville oranges - they can raise levels of some DOACs, especially rivaroxaban and apixaban. Alcohol should be limited - heavy drinking increases bleeding risk with any anticoagulant.
How do I know if my DOAC is working?
There’s no routine blood test for DOACs. You won’t know if it’s working until something happens - either a clot forms or you bleed. That’s why adherence is so critical. If you’re at high risk for clots (like after surgery or with cancer), your doctor may occasionally check anti-Xa levels, but this is rare. Focus on taking your pill every day, and report any unusual bruising, bleeding, or pain immediately.
Is one DOAC safer than the others?
Yes - but context matters. Apixaban has the lowest bleeding risk overall, especially in older adults and those with kidney issues. Dabigatran has the lowest stroke risk in AF patients. Rivaroxaban has higher GI bleeding rates. Edoxaban is often used in patients with moderate kidney impairment. Your doctor will pick based on your age, kidney function, bleeding history, and other meds. Don’t assume one is ‘best’ - the best one is the one tailored to you.
Final Thoughts: It’s Not About the Drug - It’s About You
The anticoagulant landscape has changed. DOACs are the new standard for most people. But warfarin isn’t outdated - it’s essential for specific cases. The real question isn’t ‘Which is safer?’ It’s ‘Which one lets me live without fear?’ If you’re tired of weekly blood draws, if you can’t keep a food diary, if you’ve had a scary bleed on warfarin - DOACs might be your answer. But if you have a mechanical valve, severe kidney disease, or can’t afford the cost, warfarin still has a place. The safest choice is the one you’ll take every day, without guesswork, without panic, and without regret.




David Cusack
November 21, 2025 AT 14:09Warfarin? Honestly, it’s a relic-like fax machines, but with more bleeding-and more paperwork. I mean, who in 2025 still needs monthly blood draws? DOACs? Clean, predictable, no salad-induced strokes. The fact that we’re still debating this is like arguing whether to use a slide rule or a calculator.
Willie Doherty
November 22, 2025 AT 21:09While DOACs demonstrate superior efficacy in randomized controlled trials, their real-world pharmacokinetic variability remains underappreciated. In elderly populations with polypharmacy, drug-drug interactions are not trivial, and renal clearance profiles differ significantly among agents. A 2023 JAMA Network Open meta-analysis indicates that apixaban maintains the most favorable safety profile in patients with moderate renal impairment.
Darragh McNulty
November 23, 2025 AT 03:26DOACs changed my life 😊 No more finger pricks, no more ‘did I eat spinach last night?’ panic. I’ve been on apixaban for 3 years-zero bleeds, zero stress. Warfarin was a full-time job. DOACs? Just take it and go live. 🙌
Elaina Cronin
November 24, 2025 AT 22:18It is imperative to recognize that the clinical trial data supporting DOACs does not universally translate to real-world populations, particularly those with socioeconomic barriers to medication adherence, inconsistent access to emergency care, or limited health literacy. The reduction in intracranial hemorrhage is statistically significant, yet the increased gastrointestinal risk demands careful patient selection and monitoring protocols that are often absent in under-resourced settings.
Franck Emma
November 26, 2025 AT 21:23I almost died on warfarin. One salad. One INR test. One ER trip. DOACs saved me. I’m alive because I didn’t have to count kale.
Florian Moser
November 27, 2025 AT 07:17For those considering DOACs, remember: adherence is non-negotiable. Missing a dose increases thrombotic risk more than most people realize. Apixaban’s twice-daily dosing helps with consistency-your body learns the rhythm. Don’t treat it like aspirin. It’s not.
Nikhil Purohit
November 29, 2025 AT 04:02Been on rivaroxaban for 2 years now. My grandma was on warfarin-she had 3 INR spikes in 6 months. I just take mine with breakfast and forget. No more ‘is my blood too thin?’ nightmares. DOACs are the future, no doubt. 🤘
Michael Marrale
November 30, 2025 AT 07:50Wait… did you know the FDA approved DOACs because Big Pharma bribed the regulators? Warfarin is cheaper, safer, and has been used for 70 years. They just want you hooked on $300 pills. I’ve got a cousin who got a brain bleed on apixaban. They don’t tell you that. 🤫
David vaughan
November 30, 2025 AT 09:35DOACs are great, but… what about reversal agents? Warfarin has vitamin K and PCC. DOACs? Idarucizumab for dabigatran, and andexanet alfa for factor Xa inhibitors… which cost $30K per dose. And hospitals don’t always stock them. So… are we trading one risk for another? 😔
Logan Romine
December 1, 2025 AT 08:50So we’re choosing between a 70-year-old drug that requires constant babysitting… and a new one that’s like a black box with a price tag. Maybe the real question isn’t ‘which drug?’ but ‘who gets to decide for you?’ The system doesn’t care if you live or die-it just wants you compliant. 🤷♂️
Chris Vere
December 1, 2025 AT 18:04Interesting discussion. In Nigeria, warfarin remains the only option for most due to cost and availability. DOACs are luxury items. We adapt. We monitor. We survive. The science is good, but access is justice.
Pravin Manani
December 1, 2025 AT 20:12From a pharmacokinetic standpoint, DOACs exhibit time-independent absorption and minimal CYP450 involvement, which significantly reduces variability in therapeutic response. However, the elimination half-life of dabigatran is heavily dependent on renal function, whereas apixaban’s dual hepatic and renal clearance confers greater stability in CKD stages 3–4. This is why apixaban is preferred in the elderly with eGFR 30–50.
Eliza Oakes
December 3, 2025 AT 10:49Oh please. DOACs are just a marketing scam. Warfarin is proven. DOACs? They’ve only been around 15 years. What if they cause some weird cancer in 2040? We don’t know! You’re all just sheep following the latest trend. I’m on warfarin and I’m proud of it.
Clifford Temple
December 5, 2025 AT 04:51Warfarin is American-made. DOACs? Mostly European or Japanese. Why are we letting foreign pharma dictate our healthcare? We should go back to the good ol’ US-made warfarin. It’s patriotic. And cheaper. And real.
Shawn Sakura
December 5, 2025 AT 23:53just took my apixaban today 😊 no more warfarin drama! i used to hate those blood tests so much… now i just take it with my coffee and forget about it. still a little scared of bleeding but… the docs say it’s way safer. thank god for science 🙏