
When you hear that a blood‑pressure pill can trigger a painful joint flare, you pause. thiazide diuretics gout risk is real, and understanding why helps you keep both blood pressure and uric acid in check.
What are thiazide diuretics?
Thiazide diuretics are a class of antihypertensive drugs that work by blocking sodium reabsorption in the distal convoluted tubule of the kidney. By reducing sodium and water retention, they lower blood volume and, consequently, blood pressure. The most common agents are hydrochlorothiazide (HCTZ) and chlorthalidone. First introduced in the late 1950s, thiazides remain one of the cheapest and most prescribed antihypertensives worldwide.
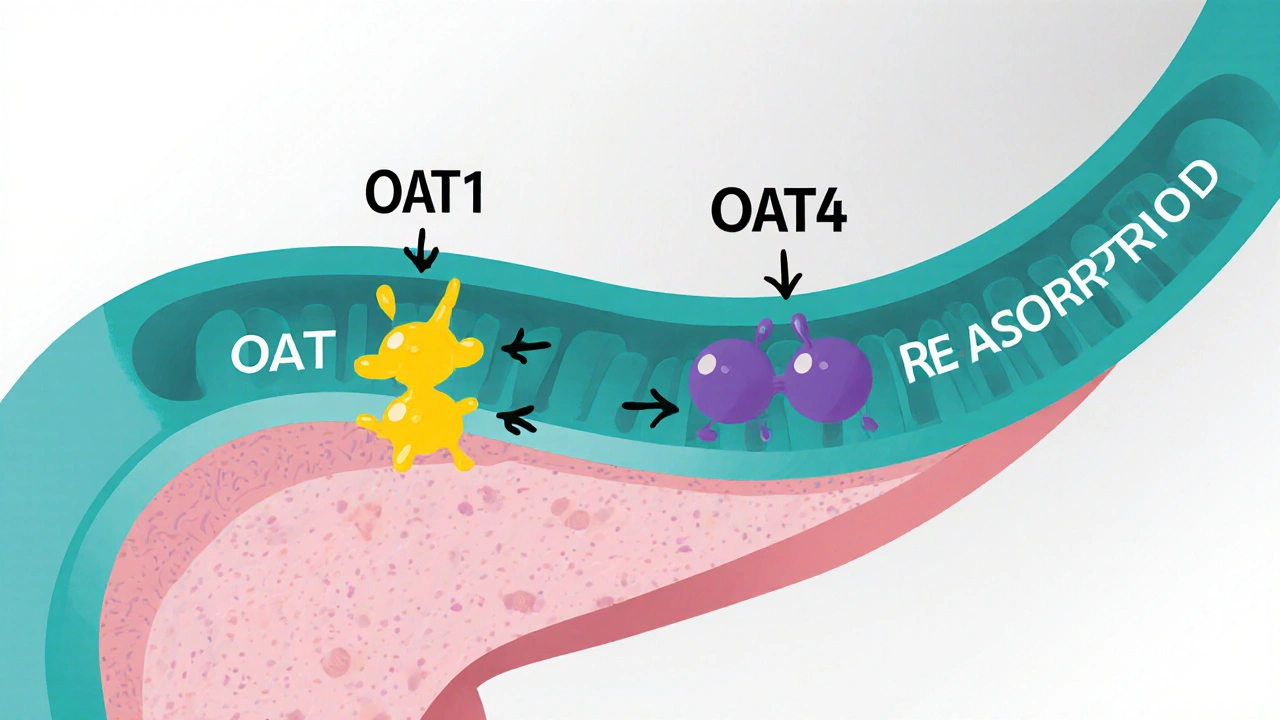
How do thiazides raise uric acid?
The link between thiazides and hyperuricemia boils down to kidney transporters. In the proximal tubule, thiazides compete with uric acid for the organic anion transporter 1 (OAT1) on the basolateral membrane and for the organic anion transporter 4 (OAT4) on the luminal side. When a thiazide molecule enters the cell, it displaces urate, prompting the kidney to re‑absorb more uric acid back into the bloodstream. The effect appears within 3‑7 days of starting therapy, is dose‑dependent, and can boost serum uric acid by 6‑21 % compared with baseline.
Gout 101: When high uric acid becomes painful
Gout is an inflammatory arthritis triggered by the deposition of monosodium urate crystals in joints, most often the first metatarsophalangeal joint (big‑toe). Serum uric acid above 6.8 mg/dL creates supersaturation, allowing crystals to form. Clinically, an acute gout flare presents as sudden, intense mono‑articular pain, swelling, and redness.
How big is the risk?
Epidemiological studies consistently show a 25‑30 % higher incidence of gout among thiazide users versus non‑users. A 2024 Nature Scientific Reports analysis reported hazard ratios rising from 1.18 in the first month of therapy to 1.41 after six months of continuous use. While only 1‑2 % of thiazide patients develop full‑blown gout, about 12‑15 % experience asymptomatic hyperuricemia, a silent precursor that can tip over with additional risk factors such as obesity, high‑purine diet, or renal insufficiency.
Who should be extra‑cautious?
- Patients with baseline serum uric acid >7.0 mg/dL (men) or >6.0 mg/dL (women).
- Anyone with a prior gout attack.
- Individuals with chronic kidney disease (eGFR <60 mL/min/1.73 m²).
- Patients on high‑dose thiazide therapy (≥25 mg HCTZ daily).
Guidelines from the American College of Cardiology (ACC) and the European Society of Cardiology (ESC) now advise measuring uric acid before initiating thiazides in these groups.
Monitoring and mitigation strategies
Below is a practical checklist you can hand to patients or use in your clinic:
- Check baseline serum uric acid.
- Re‑measure after 1‑2 weeks of starting therapy; repeat at 3 months.
- If uric acid climbs >6.0 mg/dL, consider dose reduction or switching.
- Encourage lifestyle changes: limit alcohol, reduce red meat and seafood, stay hydrated.
- For persistent elevation, add a urate‑lowering drug such as allopurinol (starting 100 mg daily) or febuxostat if allopurinol is contraindicated.
- Document any gout flares and adjust therapy promptly.
Alternative antihypertensives with neutral or beneficial uric‑acid effects
| Medication Class | Effect on Serum Uric Acid | Typical Cost (US, 2023) |
|---|---|---|
| Thiazide diuretics | ↑ 6‑21 % | $4-$6 per 90‑tablet supply |
| Losartan | ↓ modestly (URAT1 inhibition) | $15-$20 per 30 tablets |
| Calcium channel blockers | Neutral | $10-$12 per 30 tablets |
| Spironolactone (potassium‑sparing) | Neutral | $8-$10 per 30 tablets |
When a patient has both hypertension and gout, swapping to losartan or a calcium‑channel blocker can spare them the extra uric‑acid load while still controlling blood pressure.
Case vignette: Putting the pieces together
Mr. Patel, a 58‑year‑old with stage 1 hypertension, was started on 25 mg hydrochlorothiazide. His baseline uric acid was 6.4 mg/dL, borderline high. Two weeks later his serum uric acid rose to 7.5 mg/dL, and he reported a sharp, swollen toe after a weekend barbecue. The clinician halted the thiazide, started low‑dose allopurinol, and switched his antihypertensive to losartan 50 mg. Within a month his uric acid dropped to 5.9 mg/dL and his blood pressure remained controlled at 128/78 mmHg. This illustrates the “prescribing cascade” that many papers flag: a thiazide‑induced rise in uric acid leading to a second medication (allopurinol) and a drug change.
Future directions
Researchers are testing a new selective sodium‑chloride cotransporter inhibitor that appears not to interfere with OAT1 or OAT4. Early phase‑II data (2023) are promising, but results won’t be public until late 2025. Until then, clinicians must balance the cardiovascular benefits of thiazides against their gout‑provoking potential, using the monitoring tools and alternative agents outlined above.
Bottom line for patients and clinicians
- Thiazide diuretics lower blood pressure effectively but can raise uric acid.
- Risk of gout climbs with dose, duration, and pre‑existing hyperuricemia.
- Check uric acid before starting, repeat after 1-2 weeks, and act on rises.
- Consider losartan, calcium‑channel blockers, or spironolactone when gout history exists.
- If hyperuricemia persists, add allopurinol or febuxostat and counsel on diet.

Do thiazide diuretics always cause gout?
No. Only a minority (1‑2 %) of thiazide users develop clinical gout. Most experience a modest rise in uric acid that never reaches the crystal‑forming threshold.
How fast does uric acid rise after starting a thiazide?
Elevations can appear within 3‑7 days, peak around 2‑4 weeks, and stay elevated as long as the drug is continued at the same dose.
Can I stay on a thiazide if I have gout?
Yes, if you keep uric acid below 6 mg/dL. That may require lifestyle tweaks, dose adjustment, or adding a urate‑lowering drug.
Are there any cheap alternatives to thiazides that don’t raise uric acid?
Losartan is a relatively inexpensive angiotensin‑II receptor blocker that modestly lowers uric acid. Calcium‑channel blockers are also neutral, though they can be 25‑30 % pricier than generic thiazides.
Should I stop my thiazide if my uric acid spikes?
First, confirm the rise isn’t temporary (e.g., dehydration). If the level stays >6 mg/dL and you have gout risk factors, discuss dose reduction or switching with your clinician.




Sunita Basnet
October 25, 2025 AT 18:00Thiazide-induced hyperuricemia is mediated via OAT1 competition; proactive monitoring of serum urate can preempt goutogenesis; baseline uric acid stratification guides dose titration; incorporating lifestyle interventions synergizes with pharmacologic modulation; clinicians should leverage algorithmic decision support for risk mitigation.
Justin Scherer
October 25, 2025 AT 19:06Thanks for the concise summary. It’s helpful to highlight the transporter mechanism because many prescribers overlook that step. In practice I always check uric acid two weeks after initiating a thiazide and adjust if needed. Keeping the patient informed about diet and hydration can make a big difference.
Pamela Clark
October 25, 2025 AT 20:13Wow another masterpiece of medical rewriting that pretends to enlighten us about a well‑known side effect. Did you really need a 20‑paragraph essay to tell us that thiazides raise uric acid? The tables could have been a single line and the whole thing would still convey the same bland truth. I’m surprised anyone reads past the first paragraph.
Cheyanne Moxley
October 25, 2025 AT 20:46Honestly it’s appalling how often doctors push cheap diuretics without even asking about a patient’s gout history. We’re supposed to be caring professionals not profit‑driven pharmacists. If you ignore hyperuricemia you’re basically inviting pain for the sake of a few dollars saved.
Kevin Stratton
October 25, 2025 AT 22:43The relationship between blood pressure control and uric acid metabolism is a microcosm of the larger trade‑offs we constantly negotiate in medicine. When a clinician reaches for a thiazide, they are essentially choosing a weapon that offers cardiovascular protection at the cost of altering renal handling of purines. This decision is not merely biochemical; it reflects the values we place on cost, accessibility, and patient quality of life. OAT1 and OAT4, the unsung transporters, become the arbiters of whether a simple foot joint will erupt in pain. One could argue that the modest rise in serum urate is an acceptable compromise for the majority who never develop gout. Yet for the minority whose baseline uric acid hovers near the supersaturation threshold, that same rise can tip the scales dramatically. This is why a one‑size‑fits‑all prescribing policy feels philosophically uneasy. We must ask ourselves whether the pursuit of lower blood pressure justifies the introduction of a new source of suffering. From a utilitarian perspective, the net benefit may still be positive, but a deontological lens reminds us of the duty to avoid preventable harm. The emerging selective sodium‑chloride cotransporter inhibitors promise to dissolve this ethical dilemma by uncoupling antihypertensive efficacy from urate reabsorption. Until they become widely available, clinicians are left navigating a landscape of imperfect options. Pragmatically, checking a baseline uric acid level, repeating it after a short interval, and having a clear plan for escalation can mitigate risk. Lifestyle counseling-reducing red meat, limiting alcohol, and encouraging hydration-acts as a non‑pharmacologic buffer. If hyperuricemia persists, the addition of a low‑dose urate‑lowering agent is a logical, albeit incremental, step. Patient education empowers individuals to recognize early signs of a flare and seek timely care. In the end, medicine is a conversation between evidence, economics, and the lived experience of the patient. Balancing these forces with humility and curiosity is what makes the practice both challenging and rewarding 😊
Manish Verma
October 26, 2025 AT 00:06Look, we Aussies know a thing or two about cheap meds and we’re not shy about using thiazides to keep BP down. The fact that they can raise uric acid is just a minor inconvenience compared with the alternative of pricey brand‑name drugs. If you’re worried about gout, just switch to losartan or a CCB – the health system will still save a buck. Don’t let a little urate spike dictate your entire therapy plan.
Greg Galivan
October 26, 2025 AT 00:56Your optimism is cute but ignoring the data is reckless. Studies show a 25‑30% higher gout incidence among thiazide users – that’s not a "minor inconvenience". Patients with borderline uric acid can quickly cross the pain threshold. You should advise a switch before a flare hits.
Edward Brown
October 26, 2025 AT 02:53What if the pharma companies are quietly promoting thiazides because they own the cheap generics and they don’t want us to switch to losartan which is more profitable for the big pharma? The new selective inhibitor sounds promising but it’s being held back by the same interests that keep us on outdated meds. It feels like a cover up.
ALBERT HENDERSHOT JR.
October 26, 2025 AT 03:16I hear your concerns and appreciate the vigilance you bring to the discussion. While it’s true that market forces can influence prescribing patterns, the data on thiazide‑induced uric acid elevation are robust and independently verified. Encourage patients to have open conversations with their providers about alternatives, and remind them that lifestyle measures remain a cornerstone of gout prevention. Together we can navigate these complexities and empower patients to make informed choices 😊
Suzanne Carawan
October 26, 2025 AT 04:40Oh great, another reminder that cheap pills have cheap side effects.