
Missing a dose of your blood pressure pill. Forgetting your insulin. Skipping your antibiotics because you’re in a rush. These aren’t just mistakes-they’re risks. About half of all people with chronic conditions don’t take their meds as prescribed. That’s not laziness. It’s not carelessness. It’s often just human nature: busy schedules, confusing regimens, side effects, or plain forgetfulness. The good news? You don’t have to rely on sticky notes or alarm clocks anymore. Medication adherence apps are here, and they work.
Why Medication Adherence Matters More Than You Think
Skipping doses doesn’t just mean you won’t feel better. It can land you in the hospital. For people with diabetes, heart disease, or HIV, even a few missed pills can cause dangerous spikes in blood sugar, blood pressure, or viral load. The CDC estimates that non-adherence costs the U.S. healthcare system over $300 billion a year. That’s not just money-it’s lives. And it’s preventable.
Traditional tools like pill organizers help, but they don’t tell you when you missed a dose. Electronic medicine boxes like MedMinder or Hero track openings, but they cost $30 to $50 a month and need extra hardware. SMS reminders are free, but they’re easy to ignore. Apps? They do all of that-plus more-and they’re already in your pocket.
How Medication Adherence Apps Actually Work
These aren’t just alarm clocks with fancy icons. Modern medication apps combine reminders, tracking, education, and feedback into one seamless system. You enter your meds-name, dose, time, frequency-and the app sets up automatic alerts. When it’s time, your phone buzzes, plays a sound, or even sends a push notification with a picture of the pill so you know exactly what to take.
But the real power comes after the reminder. Most apps let you tap “taken” or “missed.” That data builds a personal log. Some show weekly charts. Others give you streaks, like a fitness app. You can see your progress. You can share it with your doctor. Some even warn you about dangerous drug interactions when you add a new prescription.
Apps like Medisafe and MyTherapy include educational content-short videos or articles on why your meds matter. One user with type 2 diabetes told Reddit: “After six months using Medisafe, my HbA1c dropped from 8.2 to 6.9. That’s not luck. That’s consistency.”
What Makes a Good Medication App?
Not all apps are built the same. Here’s what actually works, based on clinical studies and user feedback:
- Customizable reminders-You need to set different times for different pills. Some meds need to be taken with food. Others on an empty stomach. The best apps let you label each dose and set multiple alarms per day.
- Digital medication log-It’s not enough to get a reminder. You need to record whether you took it. This creates accountability and gives your doctor real data, not guesses.
- Progress tracking-Visual dashboards showing your adherence rate over time help motivate you. Seeing a 90% streak feels better than just hearing a beep.
- Medication interaction checker-Adding a new OTC painkiller? A good app warns you if it clashes with your blood thinner or antidepressant.
- Sync with pharmacies-Apps like Medisafe can notify your pharmacy when you’re running low and even request refills automatically.
- Security-Your health data is private. Look for apps with HIPAA compliance, end-to-end encryption, and biometric login (Face ID or fingerprint).
According to a 2025 meta-analysis in JMIR, 92% of top-performing apps include customizable reminders. Nearly 87% have dashboards. Only 64% clearly state their security practices-so check before you download.
Apps vs. Other Tools: The Real Difference
Let’s compare:
| Tool | Cost (per month) | Reminders | Tracking | Interaction Alerts | Adherence Improvement (Avg.) |
|---|---|---|---|---|---|
| Smartphone App (e.g., Medisafe) | $0-$5 | Yes, customizable | Yes, real-time | Yes | 7-40% increase |
| Electronic Pill Box (e.g., Hero) | $30-$50 | Yes, basic | Yes, only opens | No | 15-25% increase |
| SMS Reminders | $0 | Yes, generic | No | No | 10-20% increase |
| Pill Organizer | $5-$20 (one-time) | No | No | No | 5-10% increase |
Apps win because they’re not just reminders-they’re coaches. They adapt. They learn your habits. And they connect to your life, not the other way around.
Who Benefits the Most?
Studies show apps work best for people managing multiple medications daily-like those with HIV, heart failure, or diabetes. One trial found users taking nine or more pills a day improved adherence by 38% using an app. For someone on just one daily pill, the benefit is smaller but still measurable.
Age matters too. Younger users (18-45) set up apps in under 20 minutes. Older adults (65+) often need 40 minutes or more. That’s not because they’re tech-illiterate-it’s because the interface isn’t designed for them. Look for apps with large text, voice prompts, and simple navigation. Medisafe and MyTherapy both offer accessibility settings.
But apps aren’t magic. They don’t help people without smartphones. Or those with severe dementia. Or those who can’t afford data plans. In rural India, one study found minimal benefit-not because the app failed, but because the phone didn’t have signal. In the U.S., Medicaid users adopt these tools at less than half the rate of privately insured patients.
Getting Started: No Tech Expertise Needed
You don’t need to be a techie. Here’s how to start in under 15 minutes:
- Download a top-rated app: Medisafe, MyTherapy, or Round Health (all free versions available).
- Open the app and tap “Add Medication.”
- Search for your drug by name or scan the bottle’s barcode if supported.
- Enter the dose, time, and frequency (e.g., “10 mg, twice daily, with breakfast and dinner”).
- Set your alarm preferences: sound, vibration, repeat days.
- Turn on notifications and allow background alerts.
- Optional: Link to your pharmacy for refill alerts.
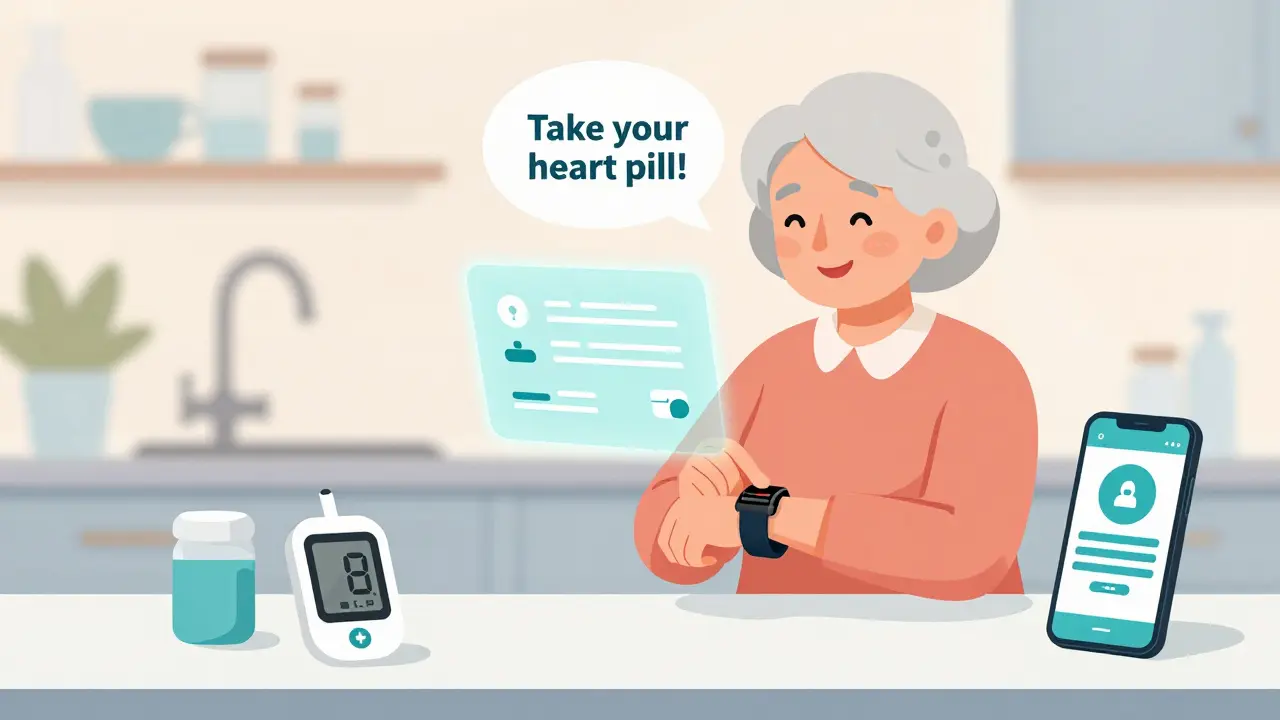
Most apps let you add photos of your pills so you know exactly what you’re taking. Some even let you assign a voice note-like “Take your heart pill” in your own voice.
Pro tip: Use your phone’s Focus Mode or Do Not Disturb to silence non-essential alerts. That way, your medication notification won’t get lost in the noise.
What Goes Wrong-and How to Fix It
People love these apps. But some quit after a few weeks. Here’s why-and how to avoid it:
- Too many notifications-If you’re getting five alarms a day, your phone feels like a nag. Reduce alerts to only essential meds. Skip reminders for vitamins or supplements unless they’re critical.
- App crashes or sync issues-Enable cloud backup. Most apps save your data online. If your phone dies, your log stays safe.
- Forgetting to mark doses-Turn on auto-log. Some apps let you say, “If I don’t tap ‘missed’ within 2 hours, assume I took it.”
- Privacy fears-Check the app’s privacy policy. Avoid ones that sell data. Stick with HIPAA-compliant apps.
One user on Capterra said: “I deleted three apps because I got so annoyed with the pop-ups. Then I found one that only alerts me once, and lets me snooze. That’s the difference.”
The Future: Smarter, Simpler, and More Connected
These apps are getting smarter. In January 2024, Medisafe launched an AI “Adherence Coach” that predicts when you’re likely to miss a dose-based on your past behavior, weather, calendar events, even your phone’s location. It nudges you before you forget.
The FDA cleared its first prescription digital therapeutic for high blood pressure in March 2024. That means doctors can now legally prescribe an app as part of your treatment plan. Some Medicare Advantage plans already cover them.
Looking ahead: Voice assistants like Google’s “Med Buddy” (coming late 2025) will let you say, “Hey Google, did I take my pill?” and get a reply. Blockchain systems are being tested to verify adherence in clinical trials without invasive monitoring.
But the real win? Integration. Soon, your app might talk to your smartwatch, your home scale, your glucose monitor. If your blood pressure spikes, your app could remind you to take your med-even if you didn’t set a reminder.
Final Thought: It’s Not About Technology. It’s About Trust.
Apps won’t fix adherence if you don’t trust your treatment. If you’re scared of side effects, confused about why you’re on five pills, or feel like your doctor doesn’t listen-no app will help. That’s why the best apps include educational content and let you share data with your care team.
Medication adherence isn’t about remembering. It’s about believing your treatment matters. And when an app helps you see your progress-when you realize you’ve taken your meds for 30 days straight-it changes everything. You start to feel in control. Not just another patient. But someone who’s managing their health.
Do medication adherence apps really work?
Yes. Fourteen randomized clinical trials from 2023 to 2025 show consistent improvements in adherence. On average, users improve their adherence scores by 7-40% compared to standard care. Apps are especially effective for people taking multiple daily doses, like those with HIV, heart disease, or diabetes.
Are medication apps free?
Most top apps-like Medisafe, MyTherapy, and Round Health-offer free versions with core features: reminders, logs, and basic tracking. Premium tiers ($4.99/month) add refill alerts, pharmacy sync, and 24/7 chat support. Free versions work well for most people.
Can I use an app if I’m over 65?
Absolutely. Many apps have accessibility features: larger text, voice-guided setup, simple menus, and voice reminders. Older users may need 20-40 minutes to set up, but once configured, they’re just as likely to stick with it. Look for apps labeled “senior-friendly” or with high ratings from users over 60.
What if I don’t have a smartphone?
Smartphone apps won’t help if you don’t have one. In that case, consider a basic electronic pill box like MedMinder or a simple alarm clock with multiple timers. Some community health centers offer free loaner devices. Ask your pharmacist or social worker-they may have options.
Can my doctor see what I take with these apps?
Only if you share it. Most apps let you export your log as a PDF or send it via email. Some, like Medisafe, connect directly to EHR systems (like Epic or Cerner) if your provider uses them. Always ask your doctor if they accept digital logs-it’s becoming more common.
Are these apps safe and private?
Reputable apps are HIPAA-compliant and use end-to-end encryption. They don’t sell your data. Look for apps that mention HIPAA, biometric login, and data encryption in their privacy policy. Avoid apps that ask for unnecessary permissions like access to your contacts or location.
How long does it take to see results?
Adherence improves within weeks. Many users report feeling more confident after just 14 days. Clinical studies show measurable improvements in health markers-like lower blood pressure or HbA1c-within 3 to 6 months of consistent use.
Next Steps: Try One This Week
Don’t wait for the perfect app. Start with the one that feels easiest. Download Medisafe or MyTherapy. Add your three most important pills. Set one reminder. Mark it taken. Do that for five days. Then add one more. You don’t need to do everything at once. Just start. Because every dose you take is a step toward better health-and apps are the quietest, most powerful tool you’ve got to help you get there.




Alvin Bregman
January 15, 2026 AT 06:47Been using Medisafe for my diabetes meds and honestly its a game changer
Sarah -Jane Vincent
January 16, 2026 AT 09:26Of course apps work. But who gave tech companies the right to monitor our pill intake like prisoners on parole? This is surveillance disguised as healthcare. Next they'll be tracking your toilet habits.
Jason Yan
January 17, 2026 AT 00:10It's not about the app. It's about the human need to be seen. When you tap 'taken' and see that streak grow, you're not just logging medicine-you're logging proof that you're still in control. That's the real magic. Not the algorithm. Not the reminders. Just you, showing up for yourself, day after day. That's the quiet rebellion against chaos.
Vicky Zhang
January 18, 2026 AT 00:24I started using MyTherapy after my mom had a stroke from skipping her blood thinner. I cried the first time I saw her 30-day streak. She didn't even know I was watching. Now she says she takes her pills because she doesn't want to break the streak. It's not about the tech-it's about giving people something to fight for. And that's beautiful.
Allison Deming
January 18, 2026 AT 07:35While the article presents a compelling narrative on medication adherence apps, it conspicuously omits the structural inequities that render such digital solutions inaccessible to vast segments of the population. The assumption that smartphones are ubiquitous, data plans affordable, and digital literacy universal is not merely optimistic-it is dangerously negligent. In rural Appalachia, in urban food deserts, in the homes of elderly Medicaid recipients without Wi-Fi, these apps are not tools-they are illusions. To celebrate technology without addressing systemic neglect is not innovation-it is performative virtue signaling.
says haze
January 19, 2026 AT 16:23Let’s be honest-this whole adherence industry is just another capitalist co-opting of vulnerability. You’re not ‘empowering’ patients-you’re monetizing their biological fragility. Gamified streaks? Achievement badges? This isn’t healthcare. It’s Fitbit for the chronically ill. And don’t get me started on the ‘AI coach’-it’s just a predictive algorithm trained on data harvested from people who can’t afford to miss work. The real solution? Universal healthcare with paid time off for medical management. But that wouldn’t generate venture capital.
Henry Sy
January 21, 2026 AT 06:06Bro I tried three of these apps and they all felt like my phone was yelling at me every 2 hours like I was a toddler. Then I found one that just says ‘hey you got a pill’ once a day and lets me snooze it. That’s all I need. No streaks no charts no fancy nonsense. Just a quiet nudge. I’ve been on track for 112 days. That’s better than any app telling me I’m a failure for missing one.
shiv singh
January 23, 2026 AT 03:03What about India? You think people in villages with no internet and phones that die after 2 hours can use this? You Americans think your apps fix everything. My cousin in Bihar takes his pills when the temple bell rings. He doesn’t need a notification. He needs food, water, and dignity. Stop selling tech as salvation.
Susie Deer
January 24, 2026 AT 23:31Why are we letting Silicon Valley run our medicine? Next they'll be selling us encrypted pill bottles with crypto rewards. This is a joke. Real Americans don't need apps to take their pills. We have willpower. We have discipline. We don't need our phones to babysit us.
Andrew Freeman
January 26, 2026 AT 15:24app works fine but my phone dies at night so i miss my 2am pill. now i just leave it plugged in next to my bed. dumb but it works. also why do they all use that same purple color? its like every med app was made by the same guy who hates yellow
Dylan Livingston
January 27, 2026 AT 04:00Oh wow, another article pretending tech can fix a system it helped destroy. You want adherence? Fix the $200 insulin. Fix the 12-hour wait for a specialist. Fix the fact that half the people reading this are choosing between meds and rent. But no-let’s just slap a progress bar on their phone and call it a win. How noble. How utterly, tragically American.
Anna Hunger
January 27, 2026 AT 06:43As a clinical pharmacist with over two decades of experience, I can confidently state that medication adherence applications have demonstrated statistically significant improvements in therapeutic outcomes across multiple chronic disease populations. The integration of behavioral psychology principles-such as positive reinforcement, self-monitoring, and goal-setting-into digital platforms represents a paradigm shift in patient engagement. Furthermore, the ability to generate longitudinal adherence reports for clinical review enhances care coordination and reduces adverse events. I strongly recommend these tools as adjunctive interventions in routine patient care.
TooAfraid ToSay
January 28, 2026 AT 06:45Let me tell you about my uncle in Lagos. He takes his meds with his morning tea. No app. No phone. Just a little plastic box his daughter brought him from America. He draws a line on the wall every time he takes it. He’s been doing it for five years. You think your app is better? Maybe. But his dignity? That’s not in your code.
Robert Way
January 29, 2026 AT 14:34so i downloaded medisafe and it asked for my contacts and my location and my calendar and i was like wait a sec but then i saw it had a feature that reminds me to drink water so i said f it i gave it everything now it tells me when to sleep too
Sarah Triphahn
January 30, 2026 AT 08:57Everyone’s acting like these apps are a miracle. But if you’re skipping your meds because you’re depressed or broke or scared of side effects, an alarm isn’t going to fix that. You need therapy. You need a doctor who listens. You need someone to hold your hand. Not a notification. Stop pretending tech can replace human care. It can’t. And pretending it can is dangerous.