Period Digestive Relief Calculator
Track Your Symptoms
Select your current digestive symptoms and cycle phase for personalized relief recommendations.
Personalized Relief Recommendations
When menstrual digestive issues refer to tummy‑ache, bloating, constipation or diarrhea that many people experience during their period, the discomfort can feel overwhelming. You might wonder why your gut decides to act up just when you’re already dealing with cramps, and more importantly, what you can actually do about it.
Why the Gut Gets Grumpy During Your Cycle
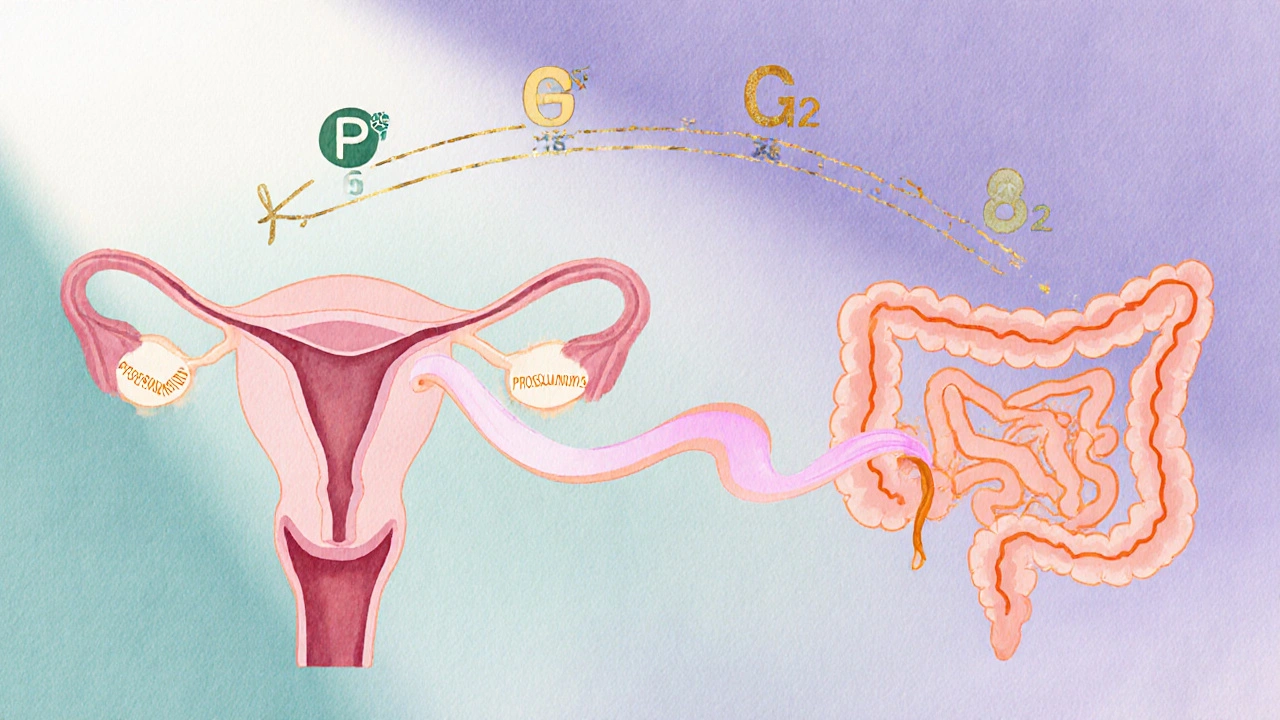
First, let’s unpack the biology. Menstruation is the monthly shedding of the uterine lining, driven by hormonal swings triggers a cascade of chemical messengers called prostaglandins. These prostaglandins, which help the uterus contract to expel its lining, also relax the smooth muscle in the intestines. The result? Slowed digestion, excess gas, or even an over‑active gut that sends you running to the bathroom.
Two key hormones-estrogen and progesterone-also play a role. In the luteal phase (the two weeks before your period), progesterone rises, which tends to slow gut motility, leading to constipation and bloating. As estrogen drops right before menstruation, that slowdown eases, sometimes flipping to diarrhea for some people.
Quick Relief Tactics You Can Try Right Now
Below are practical steps you can take the moment you feel a rumble or cramp.
- Heat therapy: Apply a warm water bottle or heating pad to your lower abdomen for 15‑20 minutes. Heat helps relax smooth muscles, easing both uterine and intestinal cramping.
- Stay hydrated: Aim for at least eight glasses of water a day. Water helps soften stool and reduces the intensity of bloating.
- Gentle movement: A short walk or simple yoga poses-like Cat‑Cow or Child’s Pose-can stimulate peristalsis and release trapped gas.
- Massage: Clockwise circular motions on your belly for a couple of minutes can promote intestinal movement.
If you need something you can sip, try a cup of peppermint tea known for its antispasmodic properties that calm intestinal muscles. A 10‑minute steep is enough; add a drizzle of honey if you like.

Food and Nutrition Tweaks to Prevent the Pain
What you eat before and during your period can make a huge difference.
- Fiber Soluble fiber (found in oats, apples, and beans) adds bulk to stool without causing excessive gas. Aim for 25‑30 grams per day, spread across meals.
- Include magnesium‑rich foods such as leafy greens, nuts, and dark chocolate, which relax muscles and may reduce cramping. A handful of almonds or a banana can be a quick snack.
- Limit salty and processed foods. Sodium encourages water retention, worsening bloating.
- Reduce caffeine and alcohol intake a few days before your period; both can stimulate the gut and worsen diarrhea.
- Try incorporating ginger fresh or powdered, which has anti‑inflammatory effects that can calm both uterine and intestinal muscles. Add sliced ginger to tea or smoothies.
Medication Options: When Home Remedies Aren’t Enough
Many people reach for over‑the‑counter (OTC) painkillers, and they can be effective-but choose wisely.
| Category | Typical Use | Pros | Cons |
|---|---|---|---|
| NSAIDs (e.g., Ibuprofen 200‑400mg every 6‑8hours) | Reduces prostaglandin production, easing cramps and bloating | Fast relief, widely available | Stomach irritation; avoid if you have ulcers |
| Antispasmodics (e.g., Dicyclomine prescription‑only, relaxes intestinal smooth muscle) | Targeted relief for severe intestinal cramping | Effective for stubborn diarrhea or constipation | Can cause dry mouth, dizziness; requires doctor’s script |
| Laxatives (e.g., Psyllium husk 1‑2tablespoons in water daily) | Prevents constipation during the luteal phase | Gentle, fiber‑based | May cause bloating if taken too quickly |
If OTC options don’t cut it, talk to a healthcare professional about prescription antispasmodics or hormonal birth control, which can steady hormone fluctuations and reduce gut symptoms.
When to See a Doctor
Digestive discomfort is common, but certain red flags mean you should get medical advice:
- Bleeding that is heavy, lasts longer than a week, or is accompanied by clotting.
- Severe abdominal pain that wakes you up at night.
- Sudden weight loss, persistent diarrhea, or stool that looks black or contains blood.
- Symptoms that interfere with daily activities for more than three cycles.
A quick visit can rule out conditions like irritable bowel syndrome (IBS), endometriosis, or inflammatory bowel disease, which sometimes flare up alongside periods.
Long‑Term Strategies for a Happier Gut
Beyond the month‑to‑month fixes, consider these habits to keep your digestive system running smoothly all year.
- Track your cycle and symptoms with a simple journal or an app. Noting foods, stress levels, and gut reactions helps you spot patterns.
- Practice stress‑reduction techniques-deep breathing, meditation, or even a short 5‑minute break during a busy day can lower cortisol, which otherwise worsens gut motility.
- Maintain regular exercise. Consistent moderate activity (like brisk walking, swimming, or cycling) supports healthy bowel movements.
- Consider probiotic supplements or fermented foods (yogurt, kefir, kimchi). A balanced gut microbiome can buffer hormonal swings.
- Stay on top of annual health checks, especially if you have a family history of gastrointestinal disorders.
These practices don’t guarantee you’ll never feel a twinge, but they build resilience so the next period feels less like a gut nightmare.
Frequently Asked Questions
Why do I get diarrhea only during my period?
The drop in estrogen just before menstruation can speed up intestinal motility, leading to looser stools. Prostaglandins also stimulate the gut, contributing to the effect.
Can birth control stop period‑related bloating?
Combined oral contraceptives steady hormone levels, which often reduces both uterine cramps and the bloating that comes from slowed digestion. Talk to your GP about the right formulation for you.
Is it safe to take ibuprofen if I have a sensitive stomach?
Take ibuprofen with food or a glass of milk to protect the lining. If you frequently experience stomach upset, ask your doctor about acetaminophen or a prescription antispasmodic instead.
What natural supplement can help with period cramps and gut pain?
Magnesium citrate, taken at 200‑400mg nightly, can relax both uterine and intestinal muscles. Many women also find ginger tea (1‑2grams of fresh ginger) soothing.
When should I consider seeing a specialist for my symptoms?
If you notice heavy bleeding, persistent severe pain, blood in stool, or symptoms that last more than three cycles, schedule an appointment with a gastroenterologist or a gynecologist for a thorough evaluation.



Erin Smith
October 12, 2025 AT 05:49Thanks for the thorough guide! I’ve tried the heat pack and a short walk, and it really helped my cramps and bloating. Keeping hydrated is easier said than done, but I’m tracking water with a phone reminder now. The tips on magnesium are great – a banana after dinner works wonders for me.
George Kent
October 14, 2025 AT 13:22Honestly, this article is a complete waste of time!!! 🙄 The so‑called ‘science’ behind probiotics is nothing but marketing hype!!! You’d think a British bloke would demand real evidence before shouting about ginger tea!!! 🍵 Stop pandering to the wellness industry and give us facts!!!
Albert Gesierich
October 16, 2025 AT 20:56While the article does cite reputable sources, it could benefit from clearer citations. For instance, the claim about prostaglandins influencing gut motility should link to a peer‑reviewed study. Additionally, the section on magnesium lacks dosage references. A more rigorous approach would strengthen credibility.
Suraj Midya
October 19, 2025 AT 04:29Thsi tip is good but you must also avoid spcy foods thrughout the luteal phase they cause extra bloated feeling.
ashish ghone
October 21, 2025 AT 12:02Hey there! I totally get how frustrating those gut swings can be during your period, and I’m glad this guide gives you some tools to fight back. First off, the heat pack is a game‑changer; I keep one by my bedside and use it whenever I feel a cramp building. Pair it with a gentle walk around the block – the movement helps push things through and eases bloating. Don’t forget to sip on peppermint tea; the menthol really calms the intestines, and a dash of honey makes it soothing. Magnesium‑rich snacks like a handful of almonds or a piece of dark chocolate can relax both uterine and gut muscles. If you’re battling constipation, a spoonful of psyllium husk mixed in water works wonders, just give it a minute to expand. Staying hydrated is key, so keep a water bottle handy and aim for at least eight glasses a day. And finally, listening to your body is the most important part – if a remedy feels off, try something else. You’ve got this! 😊
steph carr
October 23, 2025 AT 19:36I love how the article balances practical tips with the science behind them. Adding soluble fiber like oats can really keep things moving without the gas that sometimes comes from insoluble sources. Also, a quick reminder to check with your doctor before starting any new supplement, especially if you have underlying conditions. Keep up the good work!
Vera Barnwell
October 26, 2025 AT 02:09Wow, this piece really opened my eyes to the hidden drama that plays out in our guts every month. I never realized that the hormonal roller‑coaster could turn my stomach into a battlefield of bloat, cramps, and sudden dashes to the bathroom. The science behind prostaglandins acting on intestinal smooth muscle is fascinating, yet it feels like a secret conspiracy the medical community keeps under wraps. Could it be that food manufacturers are secretly capitalizing on our period‑related cravings to sell us more processed snacks? The recommendation to drink eight glasses of water sounds simple, but who has time to keep track when juggling work, school, and a social life? I’ve started a little habit of setting hourly reminders on my phone, and surprisingly, my bloating has decreased. Heat therapy is my go‑to; the warm feeling is almost meditative, and it takes the edge off both uterine and gut pain. Magnesium‑rich foods like dark chocolate feel like a treat, but they also double as a natural muscle relaxant-win‑win! Probiotic yogurt is great, but the sugar content in flavored varieties can sabotage the benefits, so plain, unsweetened options are best. I’m also curious about the role of ginger; its anti‑inflammatory properties might be the unsung hero we’ve ignored for years. The article mentions walking, yet it never addresses the fact that many of us live in snow‑bound cities where a brisk stroll is a luxury during winter months. For those of us stuck indoors, a gentle yoga flow can mimic the benefits of walking and also target the core muscles. The table comparing OTC options is helpful, but it forgets to mention that ibuprofen can irritate an already sensitive stomach if taken without food. I’d add a note to always pair NSAIDs with a small snack. Lastly, the red‑flag list is a lifesaver; recognizing when symptoms cross into dangerous territory can prevent serious health issues. Thanks for compiling all this information in one place-it feels like a secret manual for surviving period‑related gut chaos.
David Ross
October 28, 2025 AT 09:42Excellent summary of the hormonal effects on digestion; however, individual responses can vary widely, so it’s wise to experiment with the suggested strategies and adjust accordingly.
Henry Seaton
October 30, 2025 AT 17:16Heat packs work every time.
Baby Thingie
November 2, 2025 AT 00:49The recommendations are sound; consider adding a probiotic supplement. :)
Abby Elizabeth
November 4, 2025 AT 08:22Ugh, I can’t even… this article is *so* basic, like it was written by a robot who never had a period!
Mark Haycox
November 6, 2025 AT 15:56Data suggests that 73% of women experience some GI change during menstruation; however, the article fails to address underlying IBS comorbidity, which skews the overall efficacy of the suggested remedies.
Michael Taylor
November 8, 2025 AT 23:29Great job compiling all these tips, really. It’s not like anyone has been struggling with period cramps for years, right? Anyway, keep it up!
Troy Brandt
November 11, 2025 AT 07:02I’ve been curious about how diet timing influences those sudden bathroom trips during menstruation, and I think the article could expand on that angle. For example, eating a small, balanced snack with protein and complex carbs right before bed might stabilize blood sugar and reduce nighttime cramping. Also, incorporating a brief evening stretch routine could promote better digestion before sleep. It would be great to see some research references on these suggestions to back them up.
Barbra Wittman
November 13, 2025 AT 14:36Oh, because we all have endless free time to meticulously track every symptom and cross‑reference hormone charts, right? Sure, let’s all become amateur endocrinologists overnight. Meanwhile, most of us are just trying to get through the day without feeling like a balloon about to pop. But hey, if a spreadsheet helps you sleep at night, go for it. Just don’t expect the rest of us to copy‑paste your data into a color‑coded calendar.
Gena Thornton
November 15, 2025 AT 22:09If you’re looking for a quick probiotic boost, a daily serving of kefir provides both live cultures and calcium, which can help ease uterine contractions. Pair it with a 5‑minute breathing exercise to reduce stress‑induced gut sensitivity.
Lynnett Winget
November 18, 2025 AT 05:42Picture this: your belly is a bustling city, and hormones are the traffic lights. When they turn green at the right moment, everything flows smoothly; when they flick red, you get a jam of bloating. Adding a splash of turmeric to your meals can act like a friendly crossing guard, calming the rush.
Amy Hamilton
November 20, 2025 AT 13:16The cyclical nature of our bodies mirrors the seasons-each phase brings its own challenges and gifts. Embracing the digestive fluctuations as a reminder of our intrinsic connection to nature can transform discomfort into a moment of mindful awareness.
Jordan Schwartz
November 22, 2025 AT 20:49I totally hear you on the struggle to stay hydrated when you’re constantly on the go. A simple trick is to carry a reusable bottle with time markers; it makes drinking water feel like a game and keeps the bloating at bay.
Nitin Chauhan
November 25, 2025 AT 04:22Remember, consistency is key; a daily 10‑minute walk and a balanced diet will gradually train your gut to handle hormonal shifts more effectively.